Last Updated: January 02, 2023
Medically reviewed by NKF Patient Education Team
About Sepsis
Sepsis is a life-threatening emergency. It is a severe response to an infection or injury. This can include blood clots, leaky blood vessels, and drops in blood pressure. Sepsis can stop oxygen and nutrients from reaching your kidneys.
In any given year in the United States:
- At least 1.7 million adults develop sepsis
- 350,000 people die because of sepsis
- 1 in 3 patients who die in a hospital have sepsis
- Sepsis, or the infection causing sepsis, starts outside of the hospital in nearly 87% of cases
The Kidney Connection
Sepsis and kidney disease are very interrelated. Both increase the risk of causing the other.
Kidney disease can help cause sepsis.
- People on dialysis have a vascular access site under their skin and inside a blood vessel. This is known as a catheter, graft, or fistula. This access can give germs a direct way into the blood.
- Chronic kidney disease can weaken the immune system. This can raise the risk of a serious infection.
- Frequent trips to hospitals, clinics, or dialysis centers can increase your risk of getting a healthcare-acquired infection.
- Certain medications can weaken the immune system. This includes anti-rejection medicines needed after receiving a kidney transplant.
- Kidney stones can cause infections. These can also spread and lead to sepsis.
Kidney failure can also be a result of sepsis.
- Sepsis can overwhelm the body. This can cause vital organs to shut down. This usually starts with the kidneys.
- Blood pressure can drop dangerously low. This can cause less oxygen and nutrients to reach your kidneys.
- Blood clots can form within the body. This can also slow down the flow of oxygen to the kidney.
Between one third and one half of acute kidney injury cases are believed to be caused by sepsis.
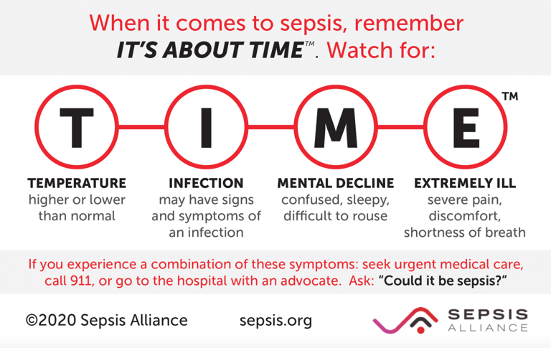
Signs and Symptoms
A person with sepsis may have any of the following symptoms:
- High heart rate or weak pulse
- Confusion or disorientation
- Extreme pain or discomfort
- Fever, shivering, or feeling very cold
- Shortness of breath
- Clammy or sweaty skin
For people on dialysis, look for signs of infection at the vascular access site. These include red skin, skin breakdown, or pus.
If you or a loved one has an infection that is not getting better or is getting worse, seek medical care immediately. This is especially true if you are having any of these symptoms. Diagnosing sepsis requires a medical assessment by a healthcare professional.
Causes
High-Risk Groups
Anyone can develop sepsis. Some people at higher risk include:
- Adults 65 years of age or older
- People with chronic medical conditions. This includes kidney disease, diabetes, lung disease, or cancer
- People with weakened immune systems. This includes people taking immunosuppressant medications and people with HIV/AIDS
- People with a recent severe illness or hospital stay
- People with a history of sepsis
- Children younger than one year of age
- Pregnant women with complications during pregnancy or childbirth
Infections
Almost any infection can lead to sepsis, especially if left untreated. Bacterial infections are the most common cause of sepsis. However, viral, fungal, and parasitic infections can also cause sepsis.
Common types or locations of infection that can lead to sepsis include:
- Appendix, abdomen, gallbladder, liver, or intestines
- Brain or spinal cord
- Pneumonia
- Cellulitis and other skin infections or wounds
- Urinary tract infections (UTIs)
Sepsis is not contagious, so it cannot spread to others. However, sepsis is usually caused by an infection, and some infections can be spread to others.
Complications
Without treatment, sepsis can cause tissue damage, organ failure, and even death. With fast recognition and treatment, most people survive without any long-term problems. Unfortunately, some people may develop permanent organ damage. This can include kidney failure, amputation, or difficulty with memory and concentration. New research also suggests severe sepsis may change a person’s immune system. This can increase the risk of infection in the future.
Post-sepsis syndrome (PSS) affects up to 50% of sepsis survivors. Examples of PSS symptoms include:
- Difficulty falling asleep or staying asleep
- Lack of energy
- Shortness of breath or difficulty breathing
- Disabling muscle or joint pain
- Swelling in your arms or legs
- Low appetite
- Hallucinations
- Panic attacks, flashbacks, or nightmares
- Loss of self-esteem
- Depression or mood swings
Diagnosis
Diagnosing sepsis requires a medical assessment by a healthcare professional. The diagnosis is based on a few different findings:
- Temperature greater than 100.4 O F (38O C) or less than 96.8 O F (36 O C)
- Systolic blood pressure less than or equal to 100. The systolic blood pressure is the top or first number of a blood pressure reading.
- Heart rate greater than 90 beats per minute
- Breathing rate greater than or equal to 22 breaths per minute
- Low O2 saturation (oxygen level in the blood)
- Difficulty breathing
Tests
In addition to the findings above, the following tests may be done to gather more information:
- Blood tests to check for signs of infection or organ damage
- Blood or other tests to identify the germ causing the infection
- An X-ray or CT scan to find an infection or organ damage
Preventing Sepsis
It is not always possible to prevent sepsis. However, here are a few tips from the CDC that can help lower your risk:
- Prevent infections
- Take care of your health
- Stay current on your recommended vaccines, especially the yearly flu vaccine
- Avoid close contact with people who have active infections that can spread
- Practice good hygiene
- Wash your hands often
- Keep cuts clean and covered until they fully heal
- Know the signs and symptoms of sepsis. (Listed in the “Signs and Symptoms” section above)
If you are on dialysis, here are some extra tips to help prevent infection:
- Clean your vascular access site well before each session
- Wash your hands before and after your dialysis session
- Wear a mask when connecting or disconnecting dialysis tubing
Nutrition
Not eating enough nutrients can lower your ability to fight infection. Ask your dietitian or healthcare provider about your nutritional needs. For general guidance, click the link that best matches your situation:
- Nutrition for people with stage 1-4 kidney disease
- Nutrition for people on hemodialysis
- Nutrition for people on peritoneal dialysis
- Nutrition for people with kidney failure
- Nutrition for children with chronic kidney disease
- Vitamins and minerals in chronic kidney disease
Exercise
Regular exercise is important for a healthy lifestyle. Remember: preventing infection is important to prevent sepsis. The following tips can help you prevent infection during exercise:
- Wear loose-fitting, moisture-wicking clothes
- Always wear shoes around pools, in locker rooms and public showers
- Disinfect gym equipment before and after using
- Wash or sanitize your hands immediately after working out
- Shower as soon as possible after exercise
- Be careful to avoid falling when possible. If you do fall, tend to any cuts or scrapes quickly
- Wear properly fitting shoes to avoid getting blisters
Visit our resource Exercise: What You Should Know for more information.
Treatment
Overview
Treatment requires urgent medical care, usually in a hospital or intensive care unit (ICU). This allows for close monitoring of your vital signs and blood tests. Treatment targets three main concerns: the sepsis, the infection causing sepsis, and any damage the sepsis caused.
Medications
Anti-infectives should be started as soon as possible. These may include antibiotics, antivirals, antifungals, or anti-parasite agents. The specific medication used will depend on the type of infection present. For example, antibiotics are used to treat bacterial infections.
Other medications are usually needed, including intravenous fluids (given through your vein). These medications can help you:
- Keep your blood pressure stable
- Prevent blood clots
- Prevent pressure ulcers
- Keep your blood sugars in target range, even if you do not have diabetes
Other
- Source Control: Removing the source of the infection as early as possible is critical. This may be an infected catheter, tube, abscess, or dead tissue in the body.
- Dialysis: If the sepsis causes acute kidney injury, dialysis can help filter toxins. This is usually stopped after the sepsis clears, and the kidneys heal. If the kidney damage is too severe, dialysis may be needed even after the sepsis clears.
- Breathing Support: Some people may need extra oxygen, a breathing tube, or a ventilator (breathing machine) to keep healthy oxygen levels.
- Artificial Nutrition: Nutrition support may have to wait until your blood pressure and fluid balance are stable. Once that happens, a feeding tube may be used to receive nutrition support. This is to avoid the infection risk with getting nutrition through a vein.
- Surgery: Sometimes surgery is needed to remove an organ or permanently damaged tissue (e.g., amputation).
Questions to ask
If you have sepsis symptoms, call 911 or go to a hospital. This is extra important if you recently had a cut, surgery, invasive procedure, or infection. Some questions to ask your healthcare team are:
- Could this infection be leading to sepsis?
- How do we know this is not sepsis?
- Should I go to the emergency room for my symptoms?
- How concerned should I be about having sepsis?
Resources
Centers for Disease Control and Prevention:
https://www.cdc.gov/sepsis/index.html
Sepsis Alliance:
https://www.sepsis.org/

















