May 12, 2020
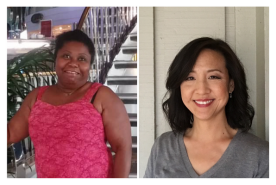
By Fiona McKinney, Kidney Patient and Kidney Advocacy Committee Member
A few weeks ago, I was interviewed for an article about “fears and concerns of contracting COVID-19 while receiving dialysis in an in-center clinic.” At the time, I said with great confidence that I had no fears because I trusted in the care of the clinic staff. My concerns centered more around the awareness that with kidney failure I have low immunity and needed to take extra safety measures while out in public, rather than the fact I was receiving dialysis at a clinic. The clinic staff practiced safety long before this crisis. They would ensure our safety now more than ever; I was certain of that.
When a fellow patient showed early signs of the virus, the clinic took immediate, pro-active measures by sending him to the ER and closing off that section of the clinic. Since I had been located right next to him, I decided to self-isolate in case I contracted something and might pass it on. I worked from home for the next few days while we waited to hear back from the hospital—an agonizing three days.
Thankfully, the patient tested negative and the clinic wasted no time establishing a new protocol for similar situations. Dialysis patients are regarded as some of most high-risk for COVID-19. The clinic immediately started checking everyone at the front door before letting anyone in. A member of staff, in full protective gear, takes everyone’s temperature. If their temperature is normal, they are given a mask and allowed into the clinic. There are no exceptions.
That was March 18th, the week before the start of the big shut down in New York City when Governor Cuomo encouraged—then insisted—that all non-essential workers work from home and businesses close.
Those few weeks seem like a lifetime ago. On April 11th, I got tested for COVID-19 after developing a persistent cough. It came on suddenly during dialysis and turned into a coughing fit that wouldn’t go away. As part of the updated clinical procedure, and knowing I was high-risk, I was sent for testing the next day and told I couldn’t return to my regular clinic for at least two weeks. If I tested positive, I would be sent to one of two clinics, neither of which appealed to me. I wondered if I would survive and knew that if I tested negative, I would still be sent elsewhere because I am symptomatic. I was regarded as a “Person Under Investigation.”
That’s when my fear and concern began to seep in. I had never thought of being at an in-center clinic as a “comfort” until I was told I would have to leave. I was terrified of the alternative. I depended so much on the people I already knew and trusted to care for me. I felt so much more vulnerable going to a place I didn’t know.
This time, test results came back within 15 hours. I was negative for the virus but still symptomatic and was told it might be a false negative. I was sent to another clinic set up only for PUIs. We were stationed at least 20 feet apart and treated late at night after the regular schedule ended (sometimes finishing at 11 p.m.) Before the two weeks were up and I could return to my regular clinic, I got chest x-rays to make sure I didn’t have COVID-pneumonia. I didn’t and the coughing fits disappeared almost as suddenly and mysteriously as they first appeared. Sadly, when I got back to my regular clinic, several older people had died from the virus. Most had been from nursing homes.
Being on dialysis is a lifelong commitment to our health and ourselves. Its many challenges–the ups and downs of treatments, the side effects and pains, the debilitating exhaustion afterwards, to name a few—seem exacerbated now. Dialysis staff taking care of us remain on the frontline of our needs—not just during COVID-19—as are the dedicated drivers taking patients back and forth to their treatments, even now. Neither gets the credit they deserve and, like us, are extra vulnerable currently. These overlooked frontline workers should be included in our praise and gratitude. As we are constantly being reminded: We are in this together.
Stay safe and be well.
From your friends at the National Kidney Foundation:
As we move forward, we need to make sure that those who need to be tested get their results quickly, rather than waiting a day or more. Dialysis patients should not need to wait for their results and risk infecting others at their dialysis centers. As we begin to bring transplantation back for those seeking a kidney, we also need to ensure they get speedy results. After all, it does little good for them, or their living organ donors, to be tested days in advance if they risk getting sick in the meantime! Please sign our recently launched petition that calls on our public leaders to ensure they’re protecting kidney patients, in part by guaranteeing they have access to COVID-19 testing.
Fiona McKinney is originally from Dublin, Ireland. She was diagnosed with Glomerulonephritis when she was 16 years old and moved to New York City in the late 1980s to seek alternative healing methods, which supported her health for over 20 years. She then became a Polarity Therapy Practitioner and teacher in private practice. In April 2008, she developed ESRD and started dialysis. She is currently Director, Community Outreach and Manager of several marathon charity programs with Achilles International, an activities based non-profit for children and adults (including veterans) with various disabilities.