What is vesicoureteral reflux (VUR)?
About 1-3% of all infants and children have a condition called vesicoureteral reflux (VUR), which means some of their urine flows in the wrong direction after entering the bladder. Some of the urine flows back up toward the kidneys and can increase the chance of developing a urinary tract infection (UTI).
UTIs that reach the kidneys can cause health problems. That's why it's important to diagnose and monitor VUR early and treat it if needed.
What causes VUR in infants and children?
Most children who have VUR are born with it, and doctors aren't sure of the cause. It appears to happen by chance. Researchers are studying inherited or genetic factors (conditions the children are born with) that may be the cause.
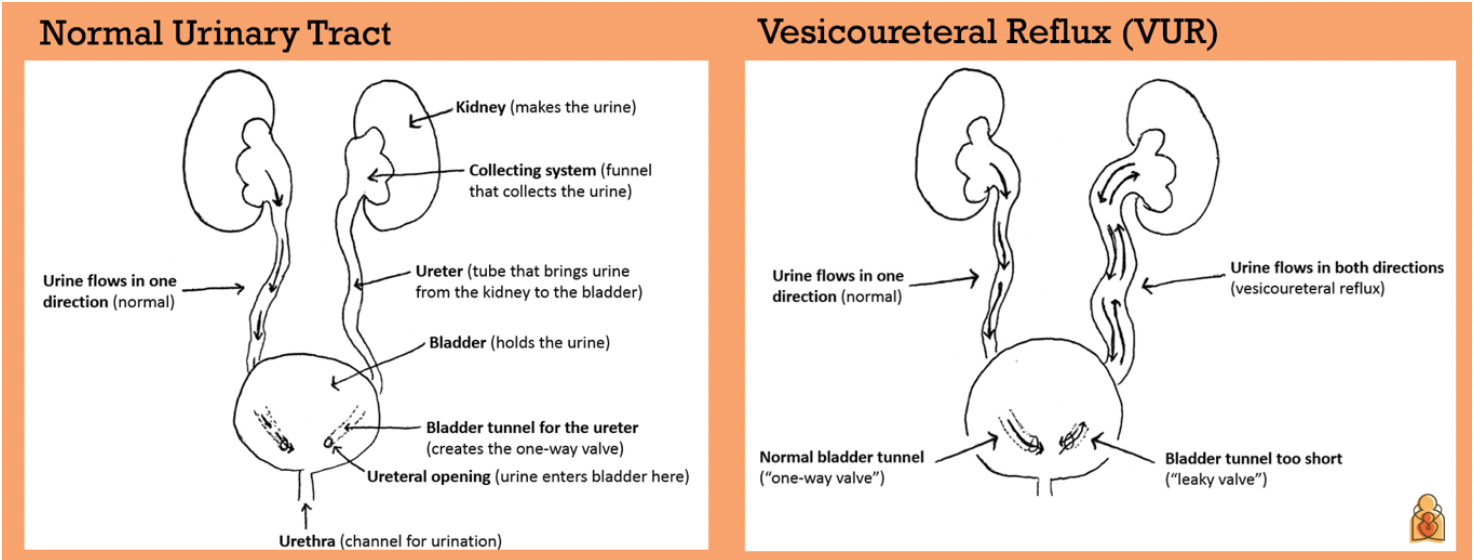
A child's urinary tract is usually a one-way street (see pictures below). The urine flows down from each kidney through tubes called ureters. The ureters enter the bladder through a tunnel of bladder muscle that creates special one-way valves to prevent urine from going back up into the kidneys. The urine in the bladder travels out of the body through another tube called the urethra.
In VUR, the tunnel in the bladder for one or both ureters may be too short, making the valve "leaky." VUR can also happen as a result of the bladder not emptying normally. This is a less common cause of VUR.
What are the signs and symptoms of VUR?
VUR doesn't usually cause symptoms until a child develops a UTI.
UTIs can be in the bladder or the kidney.
- Bladder UTI: These are common and annoying, but bladder infections are usually not harmful to long-term health. Symptoms can include having to pee a lot (frequent urination) or pain when peeing.
- Kidney UTI: VUR can increase the risk of a kidney UTI (also called pyelonephritis). This is because urine that carries germs can go backwards into the kidney. A kidney UTI can make a child very sick. The child may have high fever, chills and back pain. Kidney UTIs can scar the kidneys. In rare cases, the scarring may cause high blood pressure or reduced kidney function.
VUR may also be suspected if a child has hydronephrosis, kidney swelling caused by the build-up of fluid. This can be seen on a kidney ultrasound.
What to expect during a VCUG
A thin plastic tube called a catheter is placed into the urethra, and the bladder is filled with a special fluid that can be seen by x-ray. The test is not painful, but the child may have some stress and short-term discomfort from placing the catheter.
X-rays are taken as the bladder fills up. VUR is diagnosed if the liquid goes the wrong way up a ureter and back into a kidney.
What other tests may be done in a child with VUR?
- Ultrasound: This test uses sound waves to create an image of a child's kidneys and bladder. It is recommended for all infants and toddlers after their first UTI with a fever.
- Dimercaptosuccinic Acid (DMSA) scan: A DMSA scan can give more detail about whether kidneys have developed scars as a result of kidney UTIs. A doctor may order it if a child has had many UTIs with fever.
- Blood test: Creatinine in the blood is used to measure kidney function. The creatinine level may be too high in a child with damaged kidneys.
- Blood pressure: Blood pressure should be checked at least once a year. Children with kidney problems are at higher risk for high blood pressure.
What kinds of doctor care for children with VUR?
Pediatric specialists who care for children with VUR include:
- Pediatric nephrologists: Kidney experts who treat children with kidney problems.
- Pediatric urologists: Kidney experts who do surgery on the genital and urinary tracts (kidney, ureters, bladder) of children.
How is VUR treated?
Treatment for VUR is based on a child's age, the grade of their VUR, and whether it's causing any problems, such as a lot of UTIs. In many cases, VUR will get better on its own with age.
Treatment approaches include:
- Observation: Children with lower grades of VUR may be safely watched under their doctors' care. This usually involves regular follow-up appointments. It may include imaging tests to make sure the kidneys are growing normally. Children with VUR should have their urine tested for infection any time they develop a fever and there is no other reason for the fever, like a cold.
- Preventative antibiotics (prophylaxis): Some children are given a low dose of an antibiotic every day to decrease the risk of developing a UTI while waiting to see if they outgrow the VUR. The American Academy of Pediatrics (AAP) recommends preventative antibiotics mostly for children with higher grades of VUR (grades 3-5).
- Surgery: If VUR is severe and does not get better, or if there are repeated kidney UTIs with fever, a child may benefit from surgery that fixes the leaky valve between the bladder and the ureter. Procedures include:
- Ureteral reimplantation: The connection between the ureter and bladder is corrected so that urine flows only in one direction.
- Endoscopic injection: A substance is injected into the area where the ureter meets the bladder to prevent backward flow of urine.
These procedures are common, generally very safe, and have excellent long-term success.
What else can parents of children with VUR do?
Continue to help your child with healthy bladder and bowel habits. All potty-trained children with VUR need to work on this to help prevent UTIs.
Avoid constipation. Most children get constipated. This is common around the age of potty training when they are learning to hold their bowels. Constipation makes it harder to empty the bladder and increases the risk of a UTI. It is important to avoid or treat constipation.
Discourage "holding it." Drinking enough water and eating a high-fiber diet may prevent or treat constipation. Some children may need a gentle daily laxative. Children should have a soft bowel movement every day.
It is also important that children completely empty their bladder every 2-3 hours when they are awake. Children should avoid holding their urine for long periods. This helps keep the bladder clean and prevents UTIs.
Know the early signs of a UTI
- Fever over 100.4 degrees
- Pain or burning with urination
- Frequent urination
- Lower belly or side pain
- Vomiting
- Foul-smelling urine that does not get better after drinking more fluids
If your child has any of these symptoms, call your pediatrician. Based on test results, your pediatrician will decide whether your child needs to start treatment with an antibiotic either at home or in the hospital.
Additional Information
- Reflux Disorders in Children (National Kidney Foundation)
- Recurrent Urinary Tract Infections (UTIs) in Children (American Academy of Pediatrics)
- What is a Pediatric Nephrologist? (American Academy of Pediatrics)
- What is a Pediatric Urologist? (American Academy of Pediatrics)
Source
American Academy of Pediatrics, American Society of Pediatric Nephrology and the National Kidney Foundation Patient Education Collaborative (Copyright 2019)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.


















