- Refractory gout is a rare form of gout. This condition can be painful and serious. People with refractory gout can also have problems with the kidneys.
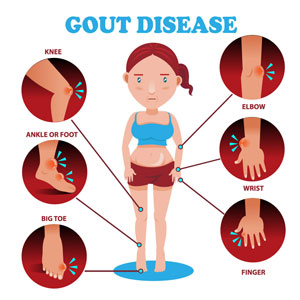
- Signs and symptoms of the disease include chronic arthritis; joints with swelling, redness, and intense pain, and tophi (lumps around hands, elbows and other body parts). The disease can continue despite treatment.
- People with refractory gout might need additional treatment to manage their disease.
Gout is a condition where a waste product called uric acid builds up in the body. Normally, uric acid dissolves in the blood, gets processed by the kidneys, and leaves the body in the urine. A small proportion of uric acid is also excreted by the intestines. With gout, there is too much uric acid in the body, either because the body makes too much uric acid, or the kidneys cannot remove as much as should.
Many things can increase the level of uric acid in the body, including certain foods, other diseases, or certain medicines. Being dehydrated (having too little water) can also increase the concentration of uric acid in the blood.
If uric acid levels in the body are too high, they may not cause problems right away. However, if uric acid levels continue to be too high over time, the extra uric acid can build up and form crystals throughout the body, especially in the joints or kidneys. In some people with gout, high levels of uric acid can go down if they lose weight or change diets. However, in people with refractory gout, this uric high acid build-up can continue.
Symptoms of gout can include:
- Joints that are swollen
- The skin around the swollen joint can be red or purple
- Pain or warmth around the joint
Gout most often happens in the joint of the big toe (called podagra), but gout can also happen to other joints in the ankles, knees, and hands. It is important to know these symptoms, because some people can have gout even if their uric acid level is normal.
With refractory gout, uric acid levels remain high and these symptoms (including painful and swollen joints) become chronic. Signs and symptoms can include
- Chronic arthritis
- Pain in a joint that becomes more intense
- Redness and swelling in a joint that gets worse
- Pain and swelling in other joints around the body
- Lumps or nodules on the hands, fingers or elbows, and other parts of the body. These are caused by hard uric acid deposits under the skin known as tophi, which can be serious, painful and disfiguring.
People with refractory gout are at higher risk for kidney stones and chronic kidney disease (when kidneys work less over time)
Gout Diagnosis
A physical exam will check for signs and symptoms related to gout. The levels of uric acid will be checked in the blood and urine. Fluid from an affected joint might also be examined for gout crystals.
If these signs and symptoms persist over time, refractory gout may be the cause.
A healthcare provider might also check for other diseases or medicines that can the increase levels of uric acid in the body.
The kidneys might also be checked. An estimate of GFR (glomerular filtration rate) is a measure how well the kidneys are working.
Imaging tests might also be used to check for kidney stones.
Treatment for Gout
Gout can be managed with dietary changes, medicine, and management of other conditions that raise uric acid levels. Most experts recommend that uric acid levels in the blood are reduced to stay below 6.0 mg/dL in order to prevent gout attacks.
Foods and drinks that contribute to uric acid and gout should be avoided. These include red meat, organ meat, seafood, beer, liquor, and sugar-sweetened items (especially with high fructose corn syrup).
Other health problems that increase the risk of gout should also be managed. These include obesity, high blood pressure, diabetes (high blood sugar), and high cholesterol. These conditions, especially diabetes and high blood pressure, can also increase the risk of kidney disease.
All medications and supplements will need to be reviewed by a healthcare provider. Some medications may also increase the uric acid levels. These include aspirin, niacin, and certain blood pressure medicines called diuretics (or water pills). Certain anti-rejection medicines that are given after a kidney transplant, (such as tacrolimus) can also raise uric acid levels. Any changes in medicines should be made by a healthcare provider.
It is important to stay well hydrated and drink enough water to help manage the symptoms of gout and reduce the risk of kidney stones. Some people have fluid restrictions due to a medical condition, such as the need for dialysis or certain heart conditions, so the amount of water or overall fluids should be discussed with a healthcare provider.
Certain medicines can also be used to lower the levels of uric acid in the body. These medicines are used to prevent future gout attacks and keep the condition from becoming chronic. Medicines used to lower uric acid levels include allopurinol (Aloprim, Lopurin, Zyloprim), febuxostat (Uloric), lesinurad (Zurampic), probenecid (Benemid) and pegloticase (Krystexxa). Allopurinol and febuxostat are considered first-line medications for preventing future gout attacks. However, with refractory gout, symptoms and high levels of uric acid (above 6 mg/dL) can continue, despite treatment. Therefore, other medicines, such as, lesinurad or probenecid might be considered for lowering uric acid levels, but they are generally not recommended for people with advanced CKD. Pegloticase is a medication available for refractory gout that is severe and does not improve with other treatments.
If you have refractory gout, all of the above steps need to be taken to help reduce uric acid levels and symptoms related to gout. If symptoms continue despite treatment, then you may need to talk to your healthcare provider about your treatment plan, and what other changes to your diet and medicines might need to be made.