Last Updated: February 21, 2025
Medically reviewed by NKF Patient Education Team
About Hematuria in Adults
Hematuria means that there’s blood in the urine. Sometimes there is a clear cause, like a kidney stone or infection. But often the cause is not known. When the cause is not known and the hematuria is transient (goes away on its own within a short time), there is usually no problem. This is more common with people who are under 35 years of age. But for people who are older than 35, hematuria may be a sign of cancer, even if it’s transient.
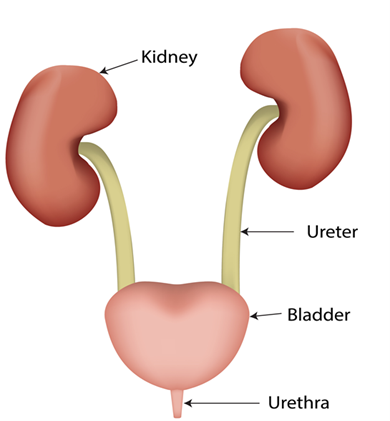
Blood can come from one or more of these places within the urinary tract (see picture below):
- Kidneys
- Ureters (tubes that connect the kidneys to the bladder)
- Bladder (where urine is stored)
- Urethra (the tube from the bladder to the outside of the body)
Signs and Symptoms
Depending on the cause, hematuria can come along with different signs and symptoms, including:
- Changes in urine color: urine may look pink, red, or the color of tea or cola
- Pain: Painful or frequent urination (going pee), or a feeling like you need to pee. Pain in the lower abdomen (belly), side, groin or back may also happen.
- Other symptoms: Nausea, vomiting, fever, and/or chills
- No symptoms: Sometimes there are no symptoms
Dark or red-colored urine does not always mean there’s blood in the urine. Certain medications, foods, or food coloring can change the color of your urine. Always talk with your doctor if you aren't sure of the cause of color changes in your urine.
Types
- Gross hematuria is when blood can clearly be seen in the toilet or in a cup. This can happen with even a small amount of blood. Large amounts of blood or clots of blood in the urine could be an emergency, so you should follow up with your healthcare provider right away.
- Microscopic hematuria is when the urine looks normal in the toilet or a cup, but blood is still present and can only be seen with a microscope. Many healthy people have microscopic hematuria that usually goes away on its own, though not always.
Causes
The most common causes of hematuria in adults include:
- Urinary tract infections
- Urinary tract inflammation (swelling)
- Kidney stones or stones in other parts of the urinary tract
Common causes in people who are over 35 years of age also include:
- Kidney cancer and bladder cancer
- Prostate cancer
- Benign prostatic hyperplasia, also known as BPH (the prostate gland grows larger than normal but is not cancerous)
Other causes include:
- Heavy exercise
- Injuries to the urinary tract or other parts of the body like the muscles
- Recent internal exams of the urinary tract (cystoscopy) or reproductive tract (pap smear)
- Menstruation (having your period)
- Endometriosis (a disease that affects the uterus)
- Sickle cell anemia (a disease passed along in families that affects red blood cells)
- Polycystic kidney disease or PKD (a disease passed along in families where balls filled with fluid grow within the kidneys)
- Glomerular disease (damage to tiny blood vessels within your kidneys’ tiny filters)
Complications
Gross hematuria that involves heavy blood loss or blood clots could mean an emergency such as:
- Large blood clots blocking urine flow out from the bladder
- Heavy bleeding that leads to low blood pressure and shock
If there is an underlying cause for the hematuria, complications can also occur if that is not treated or addressed.
Diagnosis
Tests
One or more of these tests may be done for hematuria, depending on your symptoms and the suspected cause.
Urine tests:
- Urinalysis (urine test): A test strip is placed in urine and changes color if there’s blood. This is just a screening test, so results must be confirmed by looking at the urine with a microscope.
- Urine culture: A urine test that looks for a urinary tract infection.
- Urine calcium: This test checks for high levels of calcium in the urine. High urine calcium can result in kidney stones or blood in the urine even if there are no stones.
- Urine protein: This test can help find out where the blood may be coming from. Having protein in the urine (also known as proteinuria) along with hematuria usually means there is a problem with the kidneys.
Blood tests:
- Serum creatinine: A blood test that checks how well your kidneys are filtering your blood.
- Complete blood count (CBC): A blood test that checks for anemia (not enough hemoglobin, often called red blood cells) and signs of infection (increased white blood cells).
- Complement proteins: This blood test helps diagnose some causes of a kidney disease called glomerulonephritis (inflammation of the kidney).
Other tests:
- Kidney and bladder ultrasound: An imaging test of the belly that uses painless sound waves to find cysts, kidney stones, tumors, and many other causes of hematuria.
- Kidney biopsy: This test is needed when the doctor thinks there may be damage to the filters of the kidneys. A needle is used to take a small sample of kidney tissue.
- Cystoscopy: This test looks for bleeding from the ureter, bladder, or urethra. For this test, the doctor inserts a narrow tube with a tiny camera at the end of it to look at the bladder and urethra for the cause of the hematuria.
Tests for kidney cancer and other cancers of the urinary tract:
- Computed tomography (CT) scan and/or magnetic resonance imaging (MRI) scan of the belly and pelvis without and with contrast dye
- Kidney and bladder ultrasound: An imaging test of the belly that uses painless sound waves to find cysts, kidney stones, tumors, and many other causes of hematuria.
- Cystoscopy: This test looks for bleeding from the ureter, bladder, or urethra. For this test, the doctor inserts a narrow tube with a tiny camera at the end of it to look at the bladder and urethra for the cause of the hematuria.
- Kidney biopsy: This test is needed when the doctor thinks there may be damage to the filters of the kidneys. A needle is used to take a small sample of kidney tissue.
- Urine cytology: A test that uses a microscope to look for cancer cells in the urine
Tests for prostate cancer:
- Prostate specific antigen (PSA): This measures the level in your blood of PSA, a substance that increases when prostate cancer is present
- Prostate biopsy: A small sample of prostate tissue is removed and looked at under a microscope to check for the presence of cancer cells.
Tests for Benign Prostatic Hyperplasia (BPH):
- Urinalysis (urine test): A test strip is placed in urine and changes color if there’s blood. This is just a screening test, so results must be confirmed by looking at the urine with a microscope.
- Cystoscopy: This test looks for bleeding from the ureter, bladder, or urethra. For this test, the doctor inserts a narrow tube with a tiny camera at the end of it to look at the bladder and urethra for the cause of the hematuria.
Treatment
Treatment depends on what is causing the hematuria. Often, no treatment is needed. Infections are treated with antibiotics. If there’s a high level of calcium in the urine, eating less salt and drinking more water may help. Sometimes, medication may also help lower calcium levels in the urine.
For people with glomerular disease, treatment includes medications such as steroids or other medications that decrease inflammation (swelling) in the kidney. In some people, medication is also given to reduce pressure in the kidneys and help manage high blood pressure. These medications are called ACE inhibitors and ARBs.
Kidney stones do not always need treatment but are sometimes removed if they are causing pain or infections. You may need further urine and/or blood testing to help prevent future stones.
Treatments for kidney cancer and other cancers of the urinary tract depend on the type of tumor, its location, and its stage (how much it has spread).
If all tests are normal but blood keeps showing up in the urine, yearly checkups are needed to make sure you do not begin to develop kidney disease.
Additional Information
Some medications, foods, and food colorings can cause symptoms that look like blood in the urine. Common examples include:
Foods: beets (beeturia), rhubarb, blackberries, senna (an herb)
Red food dyes like red dye 40
Medications: ibuprofen (Advil, Motrin), iron pills, nitrofurantoin (Macrodantin, Macrobid), phenazopyridine (Pyridium), rifampin, phenytoin, hydroxocobalamin (a synthetic form of vitamin B12)
Questions to ask
- Do you check my urine for blood at my yearly checkup?
- How often should my urine be checked after blood is found in my urine?
- In between checkups, what signs and symptoms should I look for after blood has been found in my urine?
- How many days should I wait after the end of my period to get an accurate test for hematuria?
- If my hematuria keeps on coming back, should I follow up with a nephrologist (kidney doctor)?

















