What is a calcium oxalate stone?
Calcium oxalate stones are the most common type of kidney stone. Kidney stones are solid masses that form in the kidney when there are high levels of calcium, oxalate, cystine, or phosphate and too little liquid. There are different types of kidney stones. Your healthcare provider can test your stones to find what type you have. Calcium oxalate stones are caused by too much oxalate in the urine.
What is oxalate and how does it form stones?
Oxalate is a natural substance found in many foods. Your body uses food for energy. After your body uses what it needs, waste products travel through the bloodstream to the kidneys and are removed through urine. Urine has various wastes in it. If there is too much waste in too little liquid, crystals can begin to form. These crystals may stick together and form a solid mass (a kidney stone). Oxalate is one type of substance that can form crystals in the urine. This can happen if there is too much oxalate, too little liquid, and the oxalate “sticks” to calcium while urine is being made by the kidneys.
Kidney Stones
Do you have chronic kidney stones?
Sign up to receive more content on kidney stones.
Who is at risk for calcium oxalate stones?
Certain risk factors may cause your body to form calcium oxalate stones. These risk factors include:
- Dehydration from not drinking enough fluid
- A diet too high in:
- Obesity
- Medical conditions like:
- Dent Disease (a rare genetic disorder that affects the kidneys)
- Hyperparathyroidism (a very high amount of a type of hormone called parathyroid hormone in the blood that causes a loss of calcium. Calcium is needed to bind with oxalate and leave the body)
- Digestive Diseases and Surgeries like:
- Inflammatory Bowel Disease (IBD) such as:
- Ulcerative Colitis
- Crohn’s Disease
- Gastric bypass surgeries
- Inflammatory Bowel Disease (IBD) such as:
It is important to know that kidney stones are more common if you have Inflammatory Bowel Disease (IBD). These conditions affect your body’s ability to absorb fats properly. When fat is not absorbed the right way, the fat binds to calcium and leaves oxalate behind. The oxalate is then absorbed and taken to the kidney, where it can form stones. Similarly, following gastric bypass surgery, your body absorbs less calcium from your digestive system. Because of this, higher levels of oxalate are found in the urinary tract. The build-up of oxalate can form crystals, which can form kidney stones.
If your calcium oxalate stones keep coming back, your healthcare provider may test you for these conditions. Your healthcare provider may also look at your lifestyle to help lower your risk factors or help find the cause of your forming calcium oxalate stones.
How can I lower my chances of forming calcium oxalate stones?
- Drink enough fluids. The number one thing you can do is to drink enough fluids, like water. Drinking enough fluids will thin out your urine and make it harder for chemicals to build up and form crystals. Your healthcare provider will look at your overall health, diet, and lifestyle and recommend the right amount of fluid you should have each day.
- Avoid eating too much protein. Eating too many foods high in protein can cause stones to form.
- Eat less salt (sodium). A diet high in salt (sodium) causes calcium to build in your urine. Too much calcium in your urine can lead to new stones. It can also cause your bones to weaken.
- Include the right amount of calcium in your diet. Some people may think they can keep stones from forming by avoiding calcium, but the opposite is true. Calcium is a nutrient that is found in dairy products, such as yogurt, milk and cheese. You need to eat calcium so that it can bind with oxalate in the stomach and intestines before it moves to the kidneys. Eating foods with calcium is a good way for oxalates to leave the body and not form stones. The best way to get calcium into your body is through the foods you eat. It may seem easier to increase your calcium by taking a supplement. However, calcium in the form of a supplement may raise your chances of forming new calcium oxalate stones. Speaking with your healthcare provider will help you find the best way to include calcium in your diet. This will help avoid having too little or too much calcium in your body.
- Avoid vitamin C supplements. Talk to your healthcare provider before taking vitamin C supplements. Too much vitamin C can cause high amounts of oxalate in the urine.
- Eat less oxalate-rich foods. Limiting how many oxalate-rich foods you eat each day may help lower your chance of forming new stones. There are some foods you should avoid because of their high oxalate levels. Some foods very high in oxalate are:
- Nuts
- Rhubarb
- Beets
- Chocolate soy milk
- All Bran®
- Buckwheat flour
- Miso
- Tahini
- Sesame seeds
- Swiss chard
Give Today
Give today and help us provide FREE resources, support, and hope for patients, loved ones and healthcare heroes.
Should I cut out all foods that have oxalate or calcium?
No, this is a common mistake. Some people think that cutting out all foods that have oxalate — or all foods with calcium — will keep stones from forming. However, this approach is not healthy. It can lead to poor nutrition and can cause other health problems. A better plan? Eat and drink calcium and oxalate-rich foods together during a meal. Doing this helps oxalate and calcium “bind” to one another in the stomach and intestines before reaching the kidneys, making it less likely for kidney stones to form in the urine.
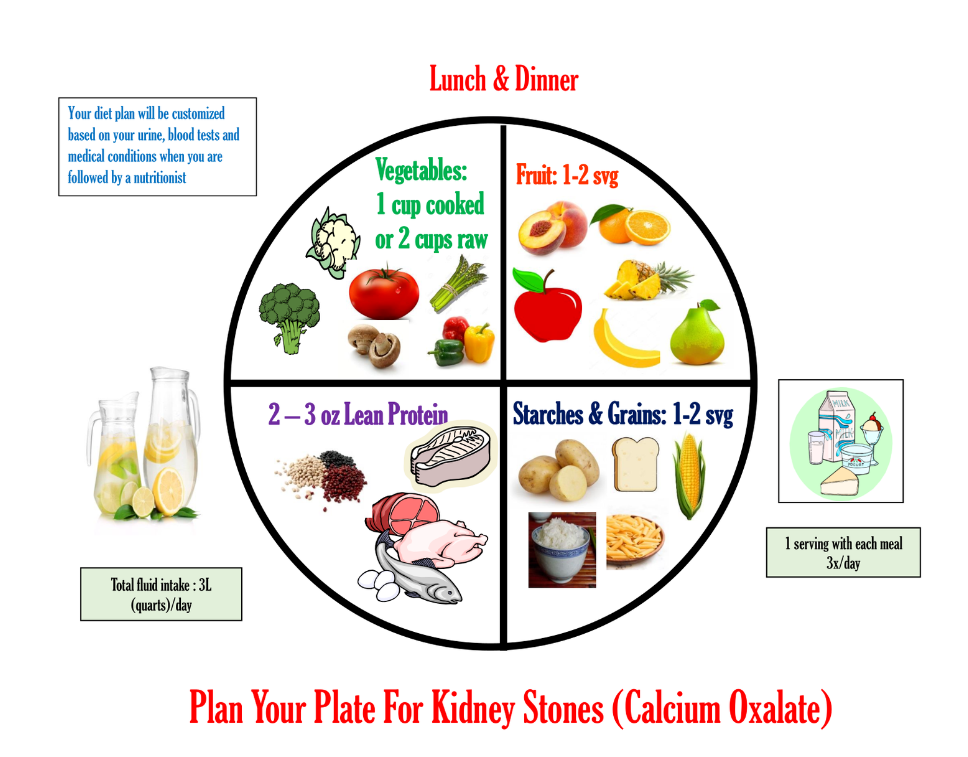
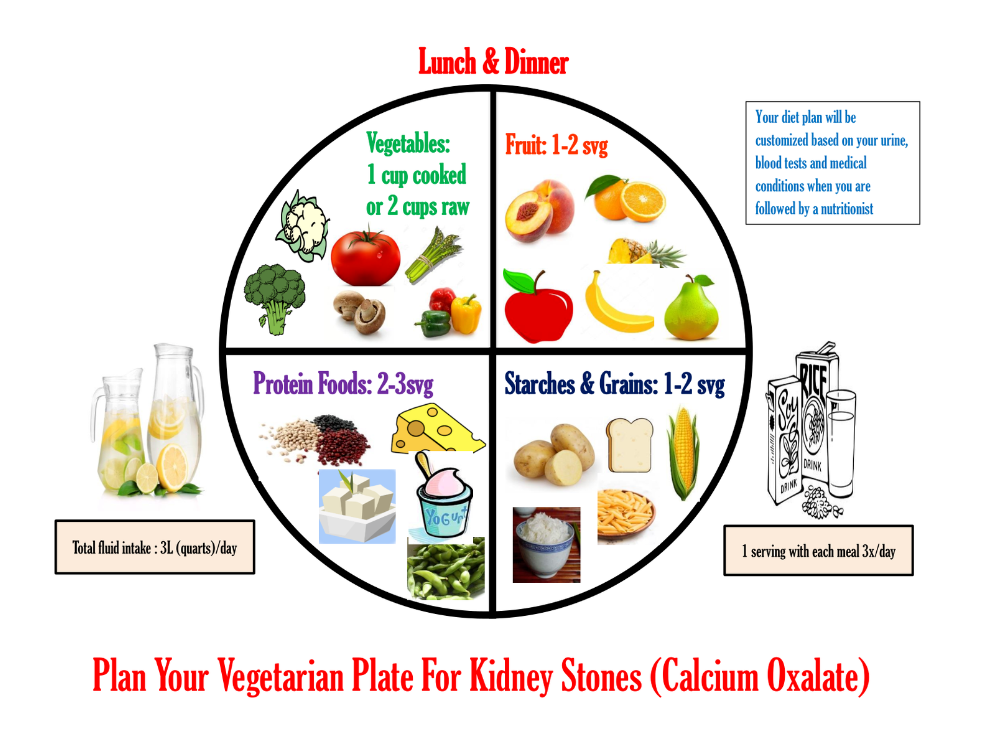
Plan Your Plate For Kidney Stones (PDF)