Chronic Kidney Disease in the Bay Area
In the nine-county Bay Area1, 430,832 Medicare beneficiaries are at-risk for CKD and of this population, less than 28% have been properly tested.
Recognizing that a community-based, multi-dimensional approach is necessary to overcome these challenges, the National Kidney Foundation (NKF) launched the Bay Area Ending Disparities in CKD Stakeholder Summit. As a part of a national NKF Collective Impact strategy, Bay Area stakeholders are implementing a roadmap to drive a cultural shift in primary care toward increasing the early diagnosis and management of CKD.
1The nine county Bay Area is defined as the following counties: Alameda, Contra Costa, Marin, Napa, San Francisco, San Mateo, Santa Clara, Solano, and Sonoma. See Land Acknowledgement below.
Land Acknowledgement
While we refer to the listed counties above as the Bay Area, we recognize that the Bay Area stands upon the ancestral and unceded territories of the Coast Miwok, Pomo, and Ohlone peoples. We recognize both the historical and ongoing injustices experienced by Indigenous communities—including the impacts of settler-colonization and genocide—as well as their resilience and achievements.
In the spirit of continuous learning and accountability, we humbly offer the following resources for further exploration:
Learning and Action Workgroups
Through a series of facilitated discussions, occurring in January through early March of 2024, leaders in health care and public health will identify barriers and solutions to improve CKD awareness, detection, and management in the Bay Area, and especially tools and strategies that can be implemented within stakeholders' own institutions. Four workgroups will convene covering the following topics:
Clinical Considerations for CKD in Primary Care
- Goal:Discuss strategies and approaches that can be employed to improve CKD recognition and care in primary care settings.
- Background:A large, national study illustrated that less than 12% of people with CKD were diagnosed in primary care.2 This included as many as 40% of people whose kidneys required specialty care. With the advent of new therapies demonstrated to slow or stop the progression of CKD, there is a very real opportunity to improve quality of care for people with CKD across the entire disease spectrum.
Community-Centered Engagement and Solutions
- Goal:Develop strategies to advance CKD awareness through community engagement and to ensure that health care providers are aware of the community resources available to delay CKD progression.
- Background:In the US today, only 10% of people with laboratory evidence of CKD know that they have kidney disease.3 Improved patient awareness, engagement, and self-management are vital to successfully slowing CKD progression. As diabetes and hypertension play significant roles in the development of CKD, working with community organizations that support people with chronic disease can be an important step toward raising public awareness of CKD among those at risk.
Policy, Payment, and Quality Measurement
- Goal:Develop a strategy to streamline CKD testing in primary care from a policy and payment perspective.
- Background:In July 2020, the NCQA released the Kidney Health Evaluation for Adults with Diabetes HEDIS measure (KHE).1 This measure assesses the percentage of people with diabetes that receive both tests for CKD during the course of a year. 2021 reporting year data shows average measure satisfaction of only 33-45% across payer types.2
Wellness and Prevention
- Goal:Develop a strategy to incorporate CKD testing and diagnosis into wellness and prevention practices within employer/ commercial health plans, and the broader community.
- Background:To date, almost 90% of people living with CKD remain undiagnosed and the majority will not receive guideline recommended annual testing.5 This workgroup will craft and propose the strategies that can be implemented to ensure that CKD testing and diagnosis are included as part of population health approaches (e.g., corporate wellness programs, disease prevention activities, payer-led prevention strategies) that are available in the Bay Area.
Meet Our Co-Chairs
Anne Davidson Barr, MBA
Managing Partner
Counterpoint Advisors, LLC
Read full bio here
Rita Nguyen, MD
Assistant State Public Health Officer
California Department of Public Health
Read full bio here
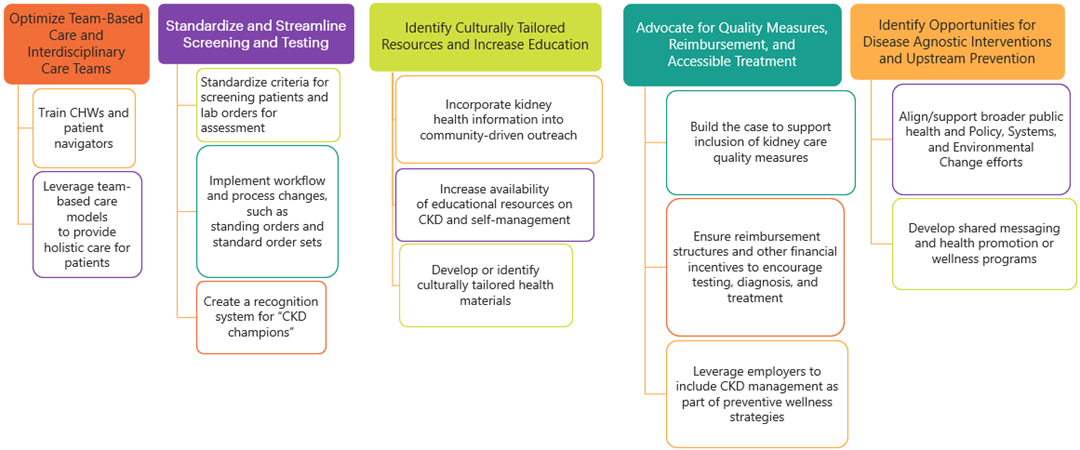
Final Roadmap
After 16 hours of facilitated discussion, 59 workgroup members representing 43 organizations, identified 13 strategies to improve testing, diagnosis, and early management of CKD in the Bay Area. Read the executive summary here.
Leadership Summit
On March 27, 2024 NKF serving CA, NV, OR, and WA hosted a virtual summit to present the final recommendations and engage partners in joining the Collective Impact Effort. 115 registered and 77 attended the live summit with 123 commitments from 32 individuals to support implementation of the 13 recommendations.
Results of the Discussions
During the learning and action workgroups, stakeholders identified several barriers to CKD testing, diagnosis, and management.
Barriers Identified:
- Lack of Systemic Focus on Preventative Health and Wellness
- Lack of Person-Centered Education and Awareness
- Structural Barriers that Disproportionately Impact Underserved Communities
- Competing Priorities in Clinical Quality Improvement
- Primary Care Capacity
Please see Executive Summary for more details regarding recommendations.
Roadmap Implementation
Disseminate NKF's CKD patient education to individuals with risk factors
In partnership with the Alameda County Community Food Bank (ACCFB), we developed an education resource (in English and Spanish) on CKD for patients who are living with diabetes. This flyer will be included in the medically tailored food boxes that ACCFB provides through CalAIM. We look forward to evaluating this pilot and are grateful to ACCFB for their partnership!
Train Community Health Workers (CHW) and Patient Navigators
According to the National Center for Farmworker Health’s (NCFH) analysis of HRSA Health Center Data from 2022, some of the most common diagnoses among agricultural workers include obesity, diabetes, and hypertension, all of which are risk-factors for CKD. With one third to half of all agricultural workers in the US residing in CA, we are customizing NKF’s current CHW training modules to better support CHWs who work with agricultural workers.
Sources:
- National Center for Farmworker Health. A Profile of Migrant Health: 2022 Analysis of HRSA Health Center Data.
- National Center for Farmworker Health. Farm Labor Data Dashboard. Date Accessed: 06 August 2024. https://ncfh.org/dashboard.html
Develop shared messaging and health promotion or wellness programs
In alignment with the California Department of Public Health’s approach to chronic disease control, the NKF is seeking opportunities to support chronic disease prevention coalitions. NKF is working to build relationships with these organizations to increase the impact of chronic disease prevention as many conditions have the same preventive measures.
Standardize criteria for screening patients and lab orders for assessment. Implement workflow and process changes, such as standing orders and standard order sets
We are connecting with health systems across the Bay Area to engage in the NKF’s Data Strategy and Learning Collaborative.
Data Strategy:
Roughly 90% of the 35.5 million US adults who have CKD are undiagnosed in primary care, despite many having laboratory evidence of CKD. Using a NKF developed framework that includes data collection and analysis, primary care practices, health systems, insurers and accountable care organizations can find gaps in CKD testing, diagnosis, and staging as part of their overall quality improvement approach to improve CKD management. Electronic Medical Record data collection and analysis not only identifies baseline measures needed to track improvement but can highlight opportunities for improvement.
Learning Collaborative:
Developed using the Institute for Healthcare Improvement Breakthrough Model, this quality improvement program provides education and guidance to clinical teams on workflow changes and clinical decision support to redesign systems and improve practice efficiency. This structured, yearlong program leverages individual clinical meetings, peer to peer engagement, didactic education and practice facilitation to drive change. Participating clinics have realized as much as 55% improvement in CKD testing and diagnosis was noted during the first year of program implementation.
Learn More and Join the Collective Impact Effort
Interested in supporting and/or participating in any of the initiatives listed above? Interested in connecting with us about a new initiative? Reach out to us!
- Nina Sherpa-Pine (she/her/hers/any pronouns used respectfully), Director of Community Impact and Health Partnerships: nina.sherpapine@kidney.org
- Mallory Caron (she/her/hers), Senior Manager Population Health Partnerships, mallory.caron@kidney.org
References
- Hanley Brown, F. Kania, J. and Kramer, M. Channeling Change: Making Collective Impact Work. Stanford Social Innovation Review. 2012. https://doi.org/10.48558/2T4M-ZR69
- Szczech, Lynda A., et al. “Primary Care Detection of Chronic Kidney Disease in Adults with Type-2 Diabetes: The ADD-CKD Study (Awareness, Detection and Drug Therapy in Type 2 Diabetes and Chronic Kidney Disease).” Public Library of Science, 26 Nov. 2014. https://doi.org/10.1371/journal.pone.0110535
- “Chronic Kidney Disease (CKD) Surveillance System: Awareness.” Centers for Disease Control and Prevention. https://doi.org/10.1371/journal.pone.0110535
- Brock, Matt. “Kidney Health: A New HEDIS Measure.” NCQA Blog, 16 Jul. 2020. https://blog.ncqa.org/kidneyhealth/
- “Chronic Kidney Disease in the United States, 2021.” Centers for Disease Control and Prevention, 4 Mar. 2021. https://www.cdc.gov/kidneydisease/pdf/Chronic-Kidney-Disease-in-the-US-2021-h.pdf