Last Updated: June 01, 2023
Medically reviewed by NKF Patient Education Team
About estimated glomerular filtration rate (eGFR)
Your kidneys filter your blood by removing waste and extra water to make urine. The best way to know how well your kidneys are filtering the blood is to look at your estimated glomerular filtration rate (eGFR). Your eGFR is calculated using your serum (blood) creatinine level, age, and sex. It can also be calculated using your cystatin C level instead of, or in addition to, your serum (blood) creatinine level.
When looking at your eGFR results, a higher number is better. In general, an eGFR value lower than 60 is a sign that your kidneys may not be working properly. An eGFR lower than 15 is a marker of kidney failure.
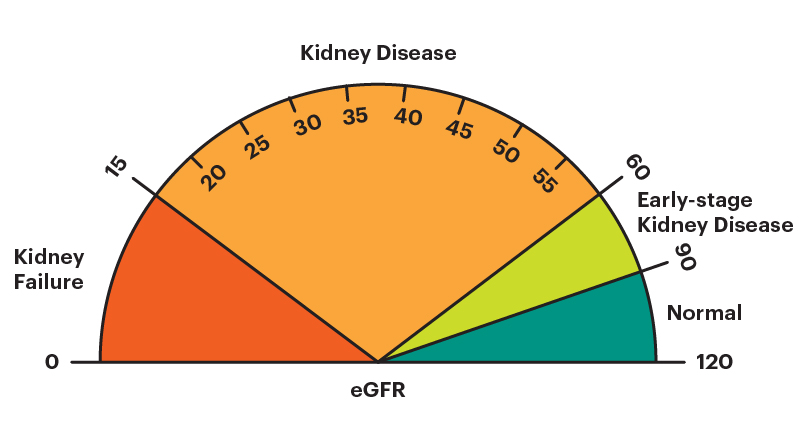
You may notice your eGFR number go up or down slightly between tests. This is normal. When trying to understand your eGFR number, it is usually better to look at the general pattern over time rather than one specific lab result.
Chronic kidney disease (CKD) versus acute kidney injury (AKI)
In general, there are two situations where your eGFR number may go down:
- Chronic kidney disease (CKD): when the kidneys become damaged over a long time. In CKD, your eGFR number goes down and stays down for 3 months or more.
- Acute kidney injury (AKI): a sudden episode of kidney failure or kidney damage that happens within a few hours or a few days. In AKI, your eGFR number goes down very quickly, but usually goes back up when the cause of the AKI is treated.
The first way to answer the question of “Can my GFR get better?” is to ask your healthcare professional whether you have AKI or CKD. Keep in mind that it is possible to have both - someone who already has CKD can still experience AKI.
After treatment, people with AKI will likely see their eGFR number go back up to where it was before their AKI episode (or be slightly lower). The damage that occurs in CKD is more permanent. So, people with CKD are less likely to see their eGFR number go up, even if it is treated.
In CKD, your eGFR number may not go back up. This does not mean there is nothing you can do to help! The information below shares some steps you can take to help prevent further kidney damage.
Engage in physical activity
Regular physical activity brings many health benefits - better blood pressure, lower stress levels, better sleep, improved muscle strength, and healthier weight. All these things can also help your kidneys stay healthy.
Stop smoking and/or using tobacco products
Using tobacco products increases your risk of high blood pressure, heart attack, stroke, and many other health problems. These products harden your blood vessels and slow the blood flow to important organs like your kidneys. This makes it harder for your kidneys to do their job. Studies also suggest that even secondhand smoke (breathing in smoke that is breathed out by people who smoke or from burning tobacco products) can increase the risk of kidney disease.
Eat a healthy and balanced diet
A healthy and balanced diet provides the right amounts of protein, carbohydrates, fats, vitamins, and minerals you need each day. There is no such thing as a one-size-fits-all “healthy diet” - everyone has different tastes and preferences. In general, a “healthy and balanced diet” that helps prevent your CKD from getting worse means eating:
- less processed foods (sugar-sweetened beverages, fast food, frozen meals, chips, candy, and pastries)
- less animal-based foods
- less sodium (salt) – aim for less than 2300 mg per day (about 1 teaspoon of salt), especially if you also have high blood pressure or heart failure
- more plant-based foods (fresh fruits and vegetables)
Be aware of diets or meal plans that promise to cure or reverse your kidney disease. Such a diet does not exist. Instead, there are diets that can help you integrate the recommendations above into your daily routine. The DASH diet is one example.
If you have more questions about how you can make your diet healthier for your kidneys, working with a kidney dietitian is a great way to get advice that is tailored specific to you.
Focus on healthy habits instead of your exact eGFR number
It is normal for your eGFR number to go down as you get older. Also, if you have chronic kidney disease (CKD), the damage that happens to your kidneys cannot be reversed. For these reasons, it is very unlikely that your eGFR number will ever go back up.
So, instead of focusing too much on your eGFR number, focus that energy on finding steps you can take to maximize your healthy habits and improve your kidney health. Taking steps now can help slow down or stop your CKD from getting worse (eGFR number going down).
One day, no one’s life will be lost to kidney disease.
- Equip patients and families with knowledge, resources, and access to high-quality care.
- Advocate for policies that address disparities and prioritize kidney health for all.
- Fund research and technology to advance early detection, improve treatment, and expand transplant access.
Keep your blood pressure and blood sugar levels within target ranges
High blood pressure and high blood sugar levels both increase the amount of stress placed on your kidneys. They can also damage the little filters that are found in your kidneys causing scar tissue and further kidney damage. This type of damage cannot be reversed. So, keeping your blood pressure and blood sugar levels within the target ranges recommended by your healthcare professional can really help your kidneys stay healthy.
Maintain a healthy weight
As your weight goes up, the amount of stress placed on your kidneys goes up too. This is especially true if you have obesity. If you are overweight or have obesity, losing weight through a balanced diet, physical activity, and sometimes medication can help keep your kidneys healthy and improve your overall health.
Consider medicines for “kidney protection”
If you have CKD, your healthcare professional may prescribe one or more medicines to help slow down or stop it from getting worse. These medicines include an ACE inhibitor/ARB, an SGLT2 inhibitor and/or an nsMRA. Sometimes a combination of these medicines may be needed.
Stay hydrated
It is important to take in enough fluids each day to keep your body hydrated. “Fluids” includes water, other liquids (coffee, tea, juice, soups, ice cream, ice cubes) and some fruits that have a lot of water in them like watermelon. Not drinking enough water makes it harder for your blood to flow to your kidneys. This puts them under extra stress as they try to do their job. Be careful - drinking too much water is not good either. So, it is important to have a balance.
There is no set rule for exactly how much water (or fluids) is “enough” for a person to drink each day. One helpful tip is to look at your urine. If it is clear or a pale-yellow color, you are likely getting enough water. If it is a darker yellow color, that may be a sign you are not getting enough water (though not always!).
If you are concerned that you might not be getting enough fluids each day, talk with your healthcare professional first before drastically increasing your intake. For example, some people with heart failure or advanced kidney disease may have a limit on how much fluid their body can handle each day.
Use non-steroid anti-inflammatory drugs (NSAIDs) with caution
These commonly used pain medicines can be harmful to your kidneys, especially at higher doses and/or with long-term use. The risk of kidney damage from NSAIDs is also higher if you are dehydrated (not taking in enough water).
Some examples of NSAIDs include:
- ibuprofen (Motrin, Advil)
- indomethacin (Indocin)
- naproxen (Aleve, Naprosyn)
- diclofenac tablets or capsules (Cataflam, Zipsor)
- celecoxib (Celebrex)
- meloxicam (Mobic)
- aspirin (only if you take more than 325 mg per day)
Many of these medicines are available over the counter and may be sold under a different name or be mixed with other ingredients (like cough & cold medicines). Sometimes it may not be possible to avoid using these products depending on your other health conditions.
If you have chronic kidney disease, always ask your healthcare professional before using any products with these drug names or if the word “NSAID” is printed on the product’s label. In general, acetaminophen, also called Tylenol, is safe for your kidneys at recommended doses - but check with your healthcare professional first to determine the cause of your pain and the best way to treat it.
Be careful when taking dietary and herbal supplements
Some dietary and herbal supplements can offer health benefits, but some can hurt much more than they help. This is true even if you do not have kidney disease. Common concerns with these products include:
- The Food and Drug Administration (FDA) does not regulate herbal supplements for dose, content, or pureness.
- Some herbal supplements have aristolochic acid, which is harmful to kidneys.
- Herbal supplements made in other countries may have heavy metals.
- Herbal supplements may interact with prescription medicines to either decrease or increase how the medicine works.
Always bring an updated list of any medications, vitamins, supplements, and herbal medicines you are taking to all your medical appointments and share it with your healthcare professional. Check with your healthcare professional or pharmacist before starting any supplements, herbal medicines, or other over-the-counter products.
Additional considerations
Remember, your eGFR number is calculated using your serum (blood) creatinine level. So, anything that causes your creatinine level to go up or down can change your eGFR number, even if it may not be related to your actual kidney health. In other words, your actual kidney function (eGFR level) may be higher or lower than what is reported in your lab results, although this is not very common.
Some factors that can lead to higher creatinine levels (making your eGFR number appear lower than it might really be) include:
- Eating large amounts of cooked meats
- Taking creatine supplements
- Recent high intensity exercise
- High muscle mass (very muscular body frame, bodybuilder)
- Taking medications such as cimetidine, cobicistat, dolutegravir, fenofibrate, ritonavir, or trimethoprim
Some factors that can lead to lower creatinine levels (making your eGFR number appear higher than it might really be) include:
- Following a vegan or vegetarian diet
- Low muscle mass
- Pregnancy
- History of an amputation or muscle wasting disease
- Severe liver disease (cirrhosis)
The actual effect that these factors may have on a person’s eGFR number is highly variable. In other words, everyone responds very differently to these factors. So, it is very important to talk with your healthcare professional if you have concerns about interpreting your eGFR number.
Preparing for Your Appointment
Questions to Ask
- Is my lower eGFR number likely because of acute kidney injury (AKI) or chronic kidney disease (CKD)?
- Are my blood pressure and blood sugar levels within my recommended goal range?
- What steps do you recommend for me to take to help keep my kidneys healthy?
- Should I be taking any “kidney protection” medications to help prevent my CKD from getting worse?
- Should I limit how much fluid I consume each day?
- Do I have any factors that might make my creatinine levels higher or lower than expected? What does this mean for how I should interpret my eGFR (kidney function) test?