November 30, 2023
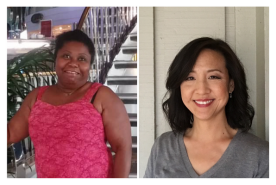
Shanaha Brown was diagnosed with kidney disease as a child. It wasn't severe, but she grew up frequenting the doctor's office to monitor the condition. For thirty-five years, Shanaha maintained her kidney function. She got married, had children, and continued living life as usual.
Shanaha's world turned upside down when she caught COVID-19. Her kidneys failed. She learned her childhood kidney disease was likely triggered by a genetic variant in her APOL1 gene, which can increase the risk of kidney disease in people with African ancestry. She received a kidney transplant from the love of her life.
This is her story.
Catching COVID-19
Shanaha and her family managed to avoid COVID-19 during its height. Once her children returned to school, it became more difficult to dodge. Despite their best efforts, the virus entered the house in November 2022.
"My daughter caught COVID-19. Since the virus can affect people with kidney disease more, she quarantined to protect me." Shanaha said, "Unfortunately, I did end up catching it, even though no one else in the house did."
Shanaha was admitted to the hospital two days before Christmas. The doctors spent the next two weeks trying to stabilize her kidney function. With limited success, they sent her home with instructions to return in a month.
"My kidney function didn't improve in January. By February, I was in kidney failure and started hemodialysis." Shanaha said, "I also learned that a kidney transplant was a future option."
While Shanaha recovered in the hospital, she wondered what her future would look like. Could she go to dialysis, work, and take care of three small children?
Kidney failure can be overwhelming and confusing, but you aren't alone. Talk to someone who's been there with NKF Peers.
Starting dialysis
[VIDEO::http://www.youtube.com/watch?v=fY7RTlhQC94::aVideoStyle]
Shanaha's fears were not unfounded. Once home from the hospital, she began home dialysis. Even though this treatment was the best option for Shanaha, it was still a challenge.
"Treatments were four days a week and took hours. I had issues with blood clotting and had to have my lines fixed three times. It was an exhausting process. It put a strain on my life but I wouldn't give up. I focused on getting a transplant," said Shanaha. "During the transplant evaluation, I learned my kidney disease was likely influenced by an APOL1 genetic variant. I never had diabetes, high blood pressure, or other risk factors. This is likely the closest answer as to what caused my kidney disease.”
During this time, loved ones near and far were going through a similar process. Except they were getting evaluated to become her living kidney donor.
"My husband Daniel was the first to get tested. He was convinced he would be a match. I didn’t think it was likely and the doctor said I'd be more likely to match with a blood family member. They didn't dissuade him from getting tested, though." Shanaha said, "On May 24th, 2023 we got the news he was a perfect match. It's incredible."
For Shanaha, learning that her husband was a match was like winning the lottery. It was the most beautiful surprise she never expected. For Daniel, it was a prayer answered.
"I prayed to God to let me be a match. I didn't want her to wait on the transplant waitlist. He answered my prayer,” said Daniel.
Are you interested in becoming a living kidney donor? Take our "Becoming a Living Donor" online course which teaches you everything you need about living kidney donation.
Getting a kidney transplant
On August 7, 2023, Daniel donated his kidney, giving Shanaha a second chance at life. Shanaha views this act of love as their second wedding and a recommitment to their love for one another.
But, what should have been a joyous occasion was soured by the staff's poor treatment of Shanaha.
"The surgery was a success but my treatment afterwards was terrible. I was in an incredible amount of pain. I asked for pain management, but the doctor called me "drug-seeking." He told me he doesn't prescribe pain medication after surgeries. He said no other patient experienced this much pain. I just had extensive surgery and no drug-seeking history. Assuming I was overstating my pain for medication is racist," said Shanaha. "When I spoke up for myself, he called me angry. It isn't okay to call a woman of color angry for standing up for herself."
The Center for Disease Control and Prevention (CDC)1 recognizes that there are long-standing disparities in pain medication within the United States. African American/Black and Hispanic people are less likely to get medicine for strong pain when they need it. Even when they are given prescription opioid drugs for pain relief, it’s at lower doses.
Shanaha, her friends, and family took these concerns to the head of the hospital. They explained that these actions were unacceptable.
"If you can't speak up for yourself, involve your family, friends, or a patient advocate. With their support, I got the help I needed," said Shanaha. "I filed a grievance as well. I wanted this on the hospital's record to help inform other patients.”

The staff offered apologies and got Shanaha the pain management she needed. Unfortunately, the insufficient care continued to stack up.
"I wasn't told about how many immunosuppressive pills I'd need every day for the rest of my life. No one told me that kidney failure patients qualify for government assistance. I learned about Medicare and The Family and Medical Leave Act on my own." Shanaha said, "I was discharged four days after the transplant. I felt discarded. Soon after, I was readmitted with a fever and excruciating pain. I was discharged only for the cycle to happen again."
Learn what to expect after a kidney transplant.
After the third discharge, Shanaha began the slow climb to recovery: "What happened to me was not okay. That’s why I’m sharing my story. I'm doing much better now. It hasn't been smooth but my health is going up instead of down."
Shanaha's kidney disease journey may not be over, but she's excited to enjoy it while spreading the joys of living kidney donation.
"I’m spreading the word to donate. There are so many people waiting who may not be as lucky as me. Know that support is available for kidney donors." Shanaha said, "For those waiting for a transplant, go to your appointments, take care of yourself, and don’t give up. You can do this."
Sharing your story like Shanaha makes all the difference! Become a Voices for Kidney Health advocate to help make change happen in government.
Support NKF's mission
Give hope and help fight kidney disease by giving a monetary gift. Your heartfelt contributions help us provide free resources, support, and hope for thousands of patients, loved ones, and healthcare heroes. Give today.
Sources
1Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. MMWR Recomm Rep 2022;71(No. RR-3):1–95. DOI: http://dx.doi.org/10.15585/mmwr.rr7103a1