Quick Reference Guide on Kidney Disease Screening
Chronic kidney disease (CKD) increases risk for all-cause mortality, cardiovascular mortality, chronic kidney failure (also called end-stage renal disease, ESRD), acute kidney injury (AKI), and other adverse outcomes. Risk for adverse outcomes can be reduced with early CKD identification and management. This online reference guide contains a 5-step plan for CKD evaluation and referral, in addition to information on glomerular filtration rate (GFR) and albumin-to-creatinine ration (ACR).
A 5-step plan for CKD evaluation and referral
- Know the criteria for CKD
- Abnormalities of kidney structure or function, present for > 3 months, with implications for health
- Either of the following must be present for > 3 months:
- Markers of kidney damage (one or more)
- GFR < 60 mL/min/1.73m2
- Recognize risk factors. CKD risk factors include, but are not limited to the following:
- Diabetes
- Hypertension
- Family history of kidney disease
- Age 60 or older (GFR declines normally with age)
- Race/U.S. ethic minority status - African Americans, Hispanics, Asians/Pacific Islanders, and American Indians
- Frequent NSAID use
- History of acute kidney injury
- Screen for CKD with two simple tests
- Spot urine for albumin-to-creatinine ratio (ACR) to detect albuminuria
- Serum creatinine to estimate glomerular filtration rate (GFR)
- Classify CKD to guide testing and treatment
- Assign GFR category
- Assign albuminuria category
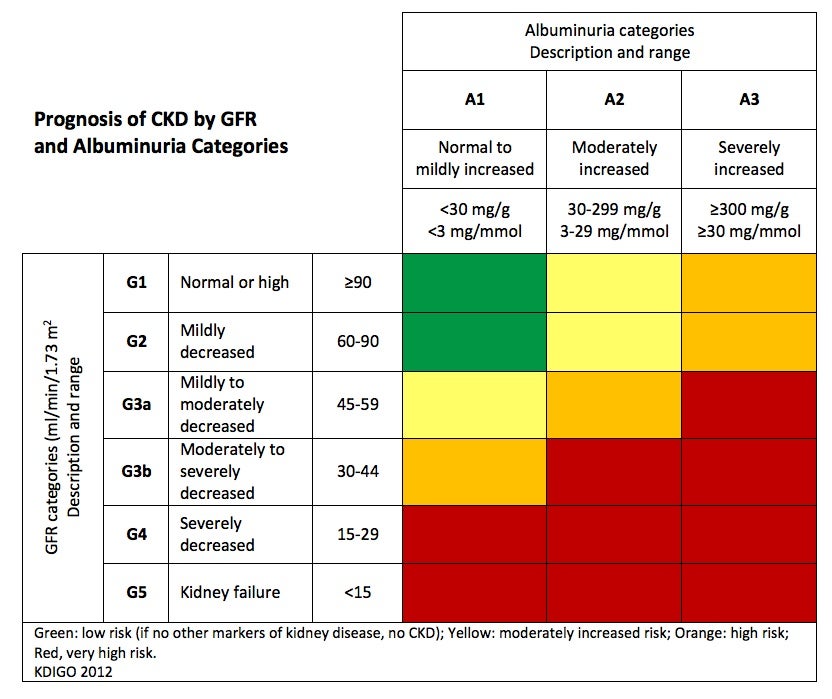
- Determine prognosis of CKD based on GFR and albuminuria category (see chart below)
- Implement a clinical action plan based on patient's CKD classification
- Consider comanagement with a nephrologist if the clinical action plan cannot be carried out
- Refer to a nephrologist when GFR < 30 mL/min/1.73 m2 or ACR > 300 mg/g
GFR
GFR as a measure for kidney function
GFR (glomerular filtration rate) is equal to the total of the filtration rates of the functioning nephrons in the kidney. GFR is considered the optimal way to measure kidney function, which in conjunction with albuminuria, can help determine the extent of CKD in an individual. The level of GFR and its magnitude of change over time are vital to:
- the detection of kidney disease
- understanding its severity (categories)
- making decisions about diagnosis, prognosis and treatment
- detection of CKD progression
A rise in blood creatinine levels is observed only after significant loss of functioning nephrons. A better way to measure kidney function is to estimate GFR with equations that use serum creatinine levels and some or all of the following variables: gender, age, weight, and race.
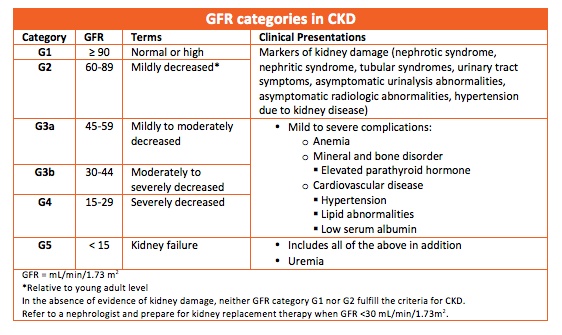
Normal GFR varies according to age, sex, and body size; in young adults it is approximately 120 ml/min/1.73 m2 and declines in normal individuals with age. However, a decrease in GFR may also be a marker of kidney disease and precedes the onset of kidney failure; therefore a persistently reduced GFR is a specific diagnostic criterion for CKD. Below 60 ml/min/1.73 m2, the prevalence of complications of CKD increases, as does the risk of cardiovascular disease (CVD). This is a 50% reduction in GFR relative to that of a young adult.
Measuring GFR
The gold standard for measuring GFR is using plasma or urinary clearance of an exogenous filtration marker. However, this is a complex procedure and generally not routinely performed. Therefore, GFR is usually estimated from the person's serum creatinine and/or cystatin C level, in combination with demographic factors such as age, race, and gender using an estimating equation.
- Use serum creatinine with age, gender, and race in the recommended CKD-EPI creatinine equation (2009).
- Use confirmatory tests in specific circumstances when eGFR based on serum creatinine is less accurate:
- Cystatin C-based equations
- Creatinie and Cystatin C-based equations
- Measured GFR
The following chart lists the GFR categories in CKD, in addition to clinical presentations associated with each category.
Calculating GFR on Smartphone and Online
- To download NKF's free GFR calculator to your smartphone: www.kidney.org/apps
- To use the free GFR calculator on the NKF website: www.kidney.org/gfr
More information on GFR
- For more information on GFR and estimating equations, visit: http://www.kidney.org/professionals/kdoqi/gfr.cfm
ACR
Albuminuria
Albuminuria is increased excretion of urinary albumin and a marker of kidney damage. Normal individuals excrete very small amounts of protein in the urine. Albumin is the most common type of protein in the urine. All patients with CKD should be screened for albuminuria. Persistent increased protein in the urine (two positive tests over 3 or more months) is the principal marker of kidney damage, acting as an early and sensitive marker in many types of kidney disease.
Detecting albuminuria
A routine dipstick is not sensitive enough to detect small amounts of urine protein. Therefore, it is recommended that screening in adults with CKD or at risk for CKD be done by testing for albuminuria.
Albumin-to-creatinine ratio (ACR) is the first method of preference to detect elevated protein. The recommended method to evaluate albuminuria is to measure urinary ACR in a spot urine sample. ACR is calculated by dividing albumin concentration in milligrams by creatinine concentration in grams.
Although the 24-hour collection has been the "gold standard," alternative methods for detecting protein excretion such as urinary albumin-to-creatinine ratio (ACR) correct for variations in urinary concentration due to hydration as well as provide more convenience than timed urine collections. The spot specimen correlates well with 24-hour collections in adults.
Definitions of abnormalities in albumin excretion
Moderately increased albuminuria, historically known as microalbuminuria, (ACR 30-300 mg/g) refers to albumin excretion above the normal range but below the level of detection by tests for total protein. Severely increased albuminuria, historically known as macroalbuminuria, (ACR >300) refers to a higher elevation of albumin associated with progressive decline in glomerular filtration rate. The following chart lists the albuminuria categories in CKD.