Last Updated: September 05, 2023
Medically reviewed by NKF Patient Education Team
Table of Contents
- About your lab values and other CKD health numbers
- Measuring your general health
- Measuring your kidney health
- Measuring your balance of important minerals and acidity
- Measuring CKD complications: nutrition & malnourishment
- Measuring CKD complications: anemia
- Measuring CKD complications: mineral and bone disorder (CKD-MBD)
- Measuring CKD complications: cardiovascular disease (CVD)
- Measuring CKD risk factors: diabetes
- Questions for your healthcare team
- More Resources
About your lab values and other CKD health numbers
It is normal to feel like living with chronic kidney disease (CKD) sometimes means you need to learn a new language. CKD is a complex condition that worsens over time. Early on, only a small number of tests may be needed. As CKD gets worse, your kidneys have a harder time doing all their jobs like helping make red blood cells, balancing important minerals, and keeping your bones healthy. So, you may notice more tests being checked and/or checked more often as your CKD gets worse. You may also need extra tests to monitor for other health conditions that are related to kidney disease.
Having regular visits with your healthcare professionals and getting your recommended lab work done can help you stay up to date with your health. But you may not be familiar with why some of these measures of your kidney-related health and wellbeing are used. So, the information below serves as a quick guide to the different types of health information that you may see in your medical record that is important for people living with CKD. Some of these tests require a blood or urine sample (also called “lab tests” or “labs”) – these are usually sent to a laboratory for measurement. Other measures, like weight or blood pressure, are usually done in an exam room.
If you have questions about your results, always talk with your healthcare professional first before taking any action.
Everybody's situation is different - some of these tests may not apply to you. Similarly, your situation may need a test that is not included in this list. Also, having test results that are not in the "normal" range (as provided on your lab sheet) doesn't always mean there is a problem or concern.
Measuring your general health
Blood pressure
A healthy blood pressure is very important for your kidneys and overall health.
- High blood pressure puts extra stress on your kidneys, heart, and blood vessels - increasing your risk for heart attack, stroke, and worsening kidney disease.
- Low blood pressure makes it hard for your blood to deliver oxygen and nutrients to all the different parts of your body. This increases your risk for acute kidney injury. It can also increase your risk for dizziness and falling.
Your blood pressure is reported as 2 separate numbers – for example “120/80” or “120 over 80”. The first/top number (called “systolic pressure”) is the pressure in your blood vessels during each heartbeat - when blood is actively pumped out of your heart to the rest of your body. The second/bottom number (called “diastolic pressure”) is the pressure in your blood vessels when your heart is resting between each beat.
The recommended blood pressure target may vary depending on factors like your age, other health conditions, risk of falling, and whether you are on dialysis. Ask your healthcare professional what your goal blood pressure should be.
Weight
Maintaining a healthy weight is important for your overall health. The definition of healthy weight depends on many other factors like your height, age, and other health conditions. So, ask your healthcare professional what a healthy body weight is for you.
- If you are underweight or losing weight without trying, you may not be getting the right nutrition to stay healthy.
- If you are overweight or slowly gaining weight, you may be getting too many calories and/or not enough physical activity.
In either of these situations, working with a dietitian can help you find ways to safely add or remove extra calories to your diet and make sure you get the right nutrition.
- Sudden weight gain can also be a serious problem, especially if you are on dialysis and/or have heart failure. It may be a sign of too much fluid in your body, especially if it also comes with symptoms like swelling, shortness of breath, and/or a rise in blood pressure.
If you are on dialysis and/or living with heart failure, it is important to ask your healthcare professional what your dry weight is – your “normal” weight without any extra fluid in your body. As part of your treatment plan, your healthcare professional may recommend weighing yourself at a certain time every day. After you check your weight, compare the number to your dry weight number. If your weight has gone up or down by too much (as defined by your healthcare professional’s directions), contact your dialysis center or clinic for further instructions.
Measuring your kidney health
Serum (blood) creatinine
Creatinine is a waste product in your blood that comes from the digestion of protein in your food and the normal breakdown of muscle tissue. It is removed from your body through the kidneys. If you have kidney disease, the kidneys can have trouble removing creatinine from your blood. So, the level of creatinine in your blood starts to go up. High creatinine levels can be a sign of acute kidney injury and/or chronic kidney disease. A “normal” creatinine level in the blood is hard to define because it can change depending on your age, sex, body size, and other factors.
Cystatin C
Cystatin C is a protein that is produced by the cells in your body. Like creatinine, it is also removed from the body through the kidneys. If you have kidney disease, the kidneys can have trouble removing cystatin C from your blood. So, the level of cystatin C in your blood starts to go up. For some people, this blood test can be helpful to measure instead of (or in addition to) your serum creatinine to check your kidney health. This test is not as common as the creatinine test and can be more expensive.
Estimated glomerular filtration rate (eGFR)
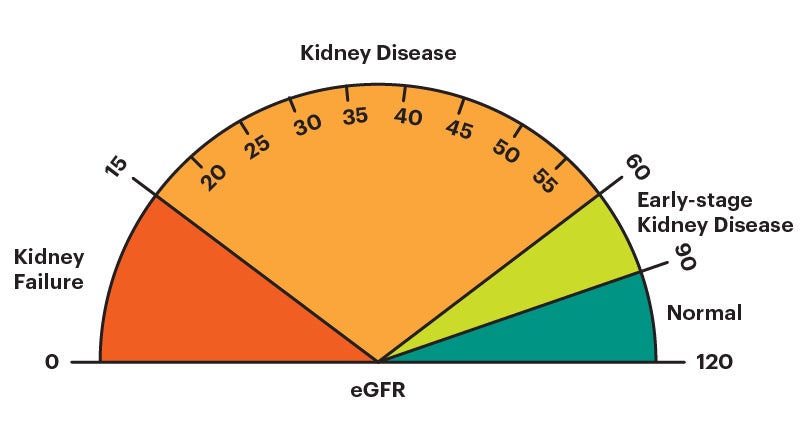
The estimated glomerular filtration rate (eGFR) is an estimate of how well your kidneys are removing waste products from the blood. It is calculated using your serum (blood) creatinine level, age, and sex. It can also be calculated using your cystatin C level instead of, or in addition to, your serum (blood) creatinine level. A “normal” eGFR varies according to age – it naturally decreases as you get older. For this test, a higher number is better.
If you have chronic kidney disease (CKD), the eGFR is used to determine your CKD stage. In general, an eGFR value lower than 60 is a sign that the kidneys may not be working properly. An eGFR lower than 15 is a marker of kidney failure.
Measured glomerular filtration rate (mGFR)
In less common situations where a more accurate measure of your kidney function is needed, your healthcare provider may order a measured glomerular filtration rate (mGFR). The mGFR is a direct measure of how well your kidneys are removing waste products from the blood. It can be a complicated and lengthy process. So, it is not used as often as the estimated GFR (eGFR).
Your healthcare professional may recommend this test if a more accurate measure of your kidney function is needed. There are many ways to complete this test – some involve collecting all the urine you make in 24 hours; others involve multiple blood samples taken from your arm over several hours. The mGFR is sometimes called a different name - measured creatinine clearance (mCrCl).
Blood urea nitrogen (BUN)
Urea nitrogen is a waste product in your blood that comes from the breakdown of protein in the foods you eat. It is removed from the body through the kidneys. A “normal” BUN level varies, and usually increases as you get older. Checking your BUN level is usually not very helpful by itself. So, your healthcare provider will likely compare your BUN level to your creatinine and eGFR levels when evaluating your kidney health.
Urine albumin-creatinine ratio (uACR)
The urine albumin-creatinine ratio (uACR) test measures the amount of two different substances in your urine (pee) – albumin (protein) and creatinine. Healthy kidneys keep the albumin in your blood while filtering the creatinine out into the urine. So, this test checks to see how well your kidneys are keeping albumin in your body and sending creatinine out.
The uACR is calculated by comparing the amount of albumin in your urine with the amount of creatinine in your urine to find the ratio. A “normal” uACR level is less than 30 mg/g. For this test, a lower number is better. A uACR level of 30 mg/g or more can be a sign of albuminuria.
When you check the results from this test on your lab report, you may see many different numbers. Focus on the result that has the word ratio in the name. For example, the name on your report may be “alb/creat ratio”, “albumin/creat ratio”, or “albumin/creat ratio, random urine”.
Urine protein-creatinine ratio (uPCR)
This test is very similar to the uACR test described above. But instead of measuring only the amount of albumin in your urine (pee), it measures all the different proteins that may be present. In some forms of kidney disease (like IgA nephropathy, lupus nephritis, or glomerulonephritis) or when testing children for protein in their urine, your healthcare professional may choose to measure your uPCR instead of uACR. A “normal” uPCR level is less than 150 mg/g. For this test, a lower number is better. A uPCR level of 150 mg/g or more can be a sign of proteinuria.
Measuring your balance of important minerals and acidity
Potassium
Potassium is an important mineral found throughout your body. It is needed for many of your body’s functions – like keeping your heart beating regularly and muscles working properly. Your kidneys help keep the right amount of potassium in the blood.
In more advanced stages of chronic kidney disease, your kidneys may have a hard time removing extra potassium from the blood, especially if you are on dialysis. People living with CKD can also be at risk for low potassium, especially during earlier stages of CKD. The recommended goal potassium level for most people is between 3.5 and 5.
Sodium
Sodium is an important mineral that helps balance the amount of fluid in your body. It also helps your nerves and muscles to work properly. Your kidneys play an active role in keeping your fluid levels balanced, partly by helping get rid of any extra sodium in your body through your urine.
In more advanced stages of chronic kidney disease, your kidneys may have a hard time balancing your fluid and blood sodium levels. This can increase your risk of high blood pressure, edema (swelling), and/or heart failure.
Having a sodium level higher or lower than the goal range can be a result of many things. So, your healthcare professional will likely compare your results from this test with your other test results (such as serum creatinine, glucose, potassium, carbon dioxide, and/or urine tests). When looked at together, your healthcare professional can provide you with custom guidance for resolving the issue (if applicable).
However, it is also possible to have a normal sodium level while still consuming too much sodium (salt). When your blood sodium level goes up, your body tries to balance it out by holding on to extra water. This is what causes symptoms like thirst, swelling, high blood pressure, and/or shortness of breath. It is important to limit your sodium (salt) intake to less than 2300 mg per day. Your healthcare professional may advise an even lower target depending on your other health conditions.
Serum (blood) bicarbonate / carbon dioxide (CO2)
Bicarbonate is needed in your blood to stop it from getting too acidic. Most of the bicarbonate in your body is in the form of carbon dioxide (CO2), a waste product from when your body turns food into energy. So, another name for this blood test is your “serum carbon dioxide (CO2)” level.
The kidneys work together with the lungs to keep your bicarbonate (carbon dioxide) level in your blood in the goal range. In more advanced stages of chronic kidney disease, your kidneys may have a hard time removing extra acidic waste products from the blood. This is also known as metabolic acidosis. A bicarbonate/CO2 level less than 22 mEq/L can be a sign your blood has too much acid – talk with your healthcare professional about a treatment plan if your labs show a CO2 (bicarbonate) level less than 22.
Measuring CKD complications: anemia
Anemia happens when you have low levels of red blood cells in your blood. Red blood cells carry oxygen from your lungs to the rest of your body. The kidneys play a very active role in helping your body make these red blood cells. Also, people living with advanced CKD can have problems absorbing iron from food. They are also at high risk for repeated blood loss from frequent blood tests and during dialysis. This makes the kidneys try to make even more red blood cells when they are having trouble keeping up in the first place. So, having a more advanced stage of chronic kidney disease increases your risk of anemia, especially for people who are on dialysis.
Keep in mind that anemia is not always caused by CKD and the descriptions below are general guides to the most common tests. If you have anemia, talk with your healthcare professional about what the primary cause may be and how you can treat it.
Measuring CKD complications: mineral and bone disorder (CKD-MBD)
Your kidneys play a very active role in balancing the ingredients needed for healthy bones – calcium, phosphorus, and vitamin D. In more advanced stages of chronic kidney disease, your kidneys may have a hard time activating vitamin D (which is needed to absorb calcium from your food) and removing extra phosphorus from the blood. This increases your risk of having calcium and phosphorus levels that are out of balance (also known as secondary hyperparathyroidism). Without close monitoring and treatment, this can cause CKD-related bone disease (also known as CKD-mineral and bone disorder or CKD-MBD).
Measuring CKD complications: cardiovascular disease (CVD)
People living with chronic kidney disease are at an increased risk of having cardiovascular disease (heart attack or stroke). This is especially true if you have an advanced stage of CKD and/or if you have albuminuria. Your risk of CVD (heart attack or stroke) is increased even more if you also have high cholesterol.
Cholesterol is a fat-like substance found throughout your body and in your blood. It is important for keeping your cells and organs healthy. Your body gets cholesterol from two places – it is absorbed from food and made in your liver. Too much cholesterol in your blood can lead to it attaching to the walls of your blood vessels, making them narrow or blocking them altogether.
A typical cholesterol test usually checks your blood for four different things:
Measuring CKD risk factors: diabetes
High blood glucose (sugar) levels over a long period of time can damage the kidneys. So, diabetes is a very strong risk factor for developing chronic kidney disease. This is especially true if your blood sugar levels are higher than your goal range for long periods of time. Two of the most common tests used to diagnose and monitor diabetes are the hemoglobin A1C and serum (blood) glucose level.
Questions for your healthcare team
- Am I at a healthy weight?
- What is my recommended goal blood pressure?
- What is my goal A1C and/or blood glucose level?
- What is my “dry weight”? What should I do if my weight at home is much higher or lower than my “dry weight”?
- Are there any test results in my lab work that you are especially concerned about or that I should pay special attention to?
- Which of my results have a different goal level or range than the “normal” range that is shared with my lab results?