About Pharmacists and Chronic Kidney Disease
Traditionally, the pharmacist’s role in caring for people living with chronic kidney disease (CKD) has been to ensure safe and effective medication use (i.e. adjusting medication doses based on a patient’s estimated kidney function).1,2 More recently, pharmacists are getting increasingly involved in broader aspects of CKD care, including screening, prevention, risk mitigation, and complication management, in collaboration with other members of the healthcare team.3–6
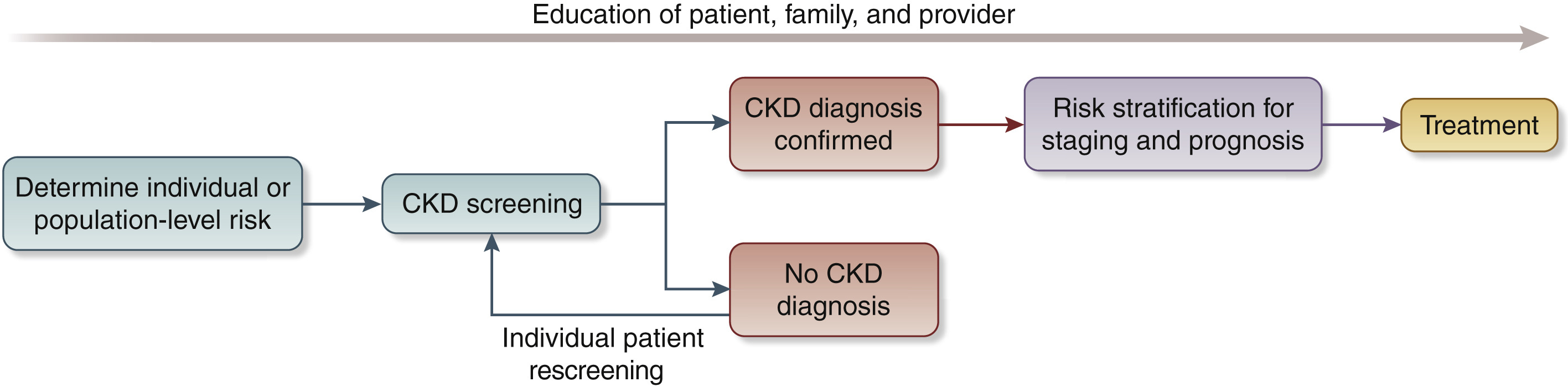
Pharmacists are well positioned to help improve overall CKD outcomes by leveraging their role and expertise at multiple steps along the CKD screening, risk stratification, treatment, and education continuum.7 Within the NKF’s CKDintercept initiative, pharmacists are recognized as essential members of the care team who support improved recognition and the effective management of early CKD and its associated cardiovascular risk.
Chronic Kidney Disease in the United States
Low recognition of CKD is a serious public health problem. Approximately 37 million Americans have CKD, representing more than 1 in 7 adults. Only 10% of people with CKD are aware of their condition. Furthermore, 1 in 3 adults in the U.S. is at risk for CKD.8
Increasing routine screening rates for people at high risk for CKD is critical and can be done with two simple laboratory tests: estimated glomerular filtration rate (eGFR) and urine albumin-creatinine ratio (uACR). Both tests are needed to obtain a complete picture of a patient’s kidney health status.9 In addition, repeat testing is usually required to confirm CKD (as opposed to acute kidney injury) and/or rule out potential false positives/negatives or other anomalies.
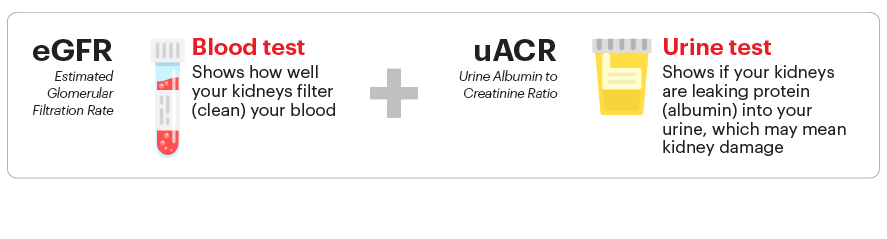
When appropriate testing occurs in a timely manner, CKD is more likely to be detected at an earlier stage when more can be done to prevent CKD progression and reduce the risk of cardiovascular events, since the two are very closely linked.10 Furthermore, albuminuria and reduced eGFR have each been shown to be independent risk factors for CKD progression and cardiovascular events/mortality, emphasizing the need for both tests.11 Lastly, the leading cause of death among people living with CKD is cardiovascular disease, so while preventing CKD progression is important, a similar focus on reducing cardiovascular risk is also essential.10

Removing Race from eGFR Equations and CKD Care
In 2020, the National Kidney Foundation (NKF) and the American Society of Nephrology (ASN) established a Task Force to reassess the inclusion of race in the estimation of GFR and its implications for diagnosis and management of patients with, or at risk for, kidney diseases.12 Race is a social construct, not a biological one, and its use in calculating a patient’s eGFR does not improve test accuracy or kidney disease management. In fact, it perpetuates kidney health inequity and adversely impacts diagnosis and treatment, particularly in advanced stages of CKD.
Many labs have made the switch to the Task Force-recommended CKD-EPI 2021 creatinine equation refit without the race variable to calculate eGFR.13 However, some laboratories continue to use the older CKD-EPI 2009 creatinine or MDRD equation, both of which include an adjustment for race. If you are working with a laboratory that has not yet implemented the race-free equation, consider initiating a conversation about making the switch. Additionally, there is an online calculator available to calculate eGFR in adults using any of the race-free equations.
Tools and Resources for Pharmacists
The following resources can be incorporated by pharmacists in their practice to support improved testing and early management of CKD.
Clinical Practice Resources
- National Kidney Foundation, 2023, How to manage CKD algorithm
- Kidney Int, 2024, KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease
- Kidney Int, 2023, Trends and perspectives for improving quality of CKD care: conclusions from a KDIGO Controversies Conference
- Kidney Int, 2021, The case for early identification and intervention of CKD: conclusions from a KDIGO Controversies Conference
Operational Resources
- National Kidney Foundation, CKD Change Package 2023: Population health strategies for cardiovascular and kidney disease risk reduction
- National Kidney Foundation, 2023, CKD screening tool for community pharmacies
Estimating GFR
- National Kidney Foundation, 2022, Frequently asked questions about GFR estimates
- N Engl J Med, 2021, New creatinine- and cystatin C-based equations to estimate GFR without race
- Am J Kidney Dis, 2021, A unifying approach for GFR estimation: Recommendations of NKF-ASN Task Force on reassessing the inclusion of race in diagnosing kidney disease
- Clin Chem, 2021, NKF Laboratory Engagement Working Group recommendations for implementing the CKD-EPI 2021 race-free equations for eGFR: practical guidance for clinical laboratories
Calculators
- Estimating GFR in adults
- Estimating GFR in pediatrics
- Kidney Failure Risk Equation
- Pediatric CKD Risk Calculator
- Predicting Risk of cardiovascular disease EVENTs (PREVENT™ calculator)
Additional Resources
- CKDintercept - a groundbreaking initiative from the National Kidney Foundation to improve chronic kidney disease testing, recognition, and management in primary care.
- Prev Chronic Dis, 2020, Public health and pharmacy: collaborative approaches to improve population health
- Centers for Disease Control and Prevention, 2017, Increasing the Use of Collaborative Practice Agreements Between Prescribers and Pharmacists: A Brief for Decision Makers, Public Health Practitioners, and Prescribers
Tools and Resources for Patients
Patients also need information and tools to understand their condition and build the motivation to set and achieve goals to protect their kidney health. The NKF can help here, too. Pharmacists can refer patients to Kidney Pathways, an online resource to help patients understand their condition and steps they can take to slow or stop its progression. This site uses a very brief questionnaire to help patients interact with their own lab results so they can access a custom course that walks them through important topics in plain language.
Educational Resources for Patients About CKD
- How your kidneys work
- Are you at risk for chronic kidney disease (CKD)?
- 6 steps to prevent kidney disease
- 7 ways to help manage chronic kidney disease (CKD)
- Exercise: what you should know
- Good nutrition
- Stages of chronic kidney disease (CKD)
- Your kidney numbers and the CKD heat map
- Estimated glomerular filtration rate (eGFR)
- Urine albumin-creatinine ratio
Educational Resources for Patients About CKD
Below is a comprehensive inventory of tools and resources pharmacists can use when interacting with patients:
- A to Z Health Guide
- Patient Education Library: Brochures
- Patient Education Library: 2-Sided Flyers
- Patient Education Library: Infographics
- Patient Education Library: Videos
Many of these valuable resources are also available in Spanish with some of the 2-sided flyers additionally available in Arabic, Bosnian, Dari, Farsi, Kinyarwanda, Nepali, Pashto, Somali, Swahili, and Vietnamese.
Other Patient Resources
- NKF Cares is our Patient Help Line, offering support for people affected by kidney disease, organ donation or transplantation. Patients, family members and caregivers can speak with a trained professional ready to answer questions and address concerns. Support, assistance, and resources are provided in English and Spanish. The toll-free phone number is 1-855-NKF-Cares (855.653.2273) or email nkfcares@kidney.org.
- NKF Peers is a national, telephone-based peer support program that connects people who want support with someone who has been there before. This program is designed to help people adjust to living with stage 4 or 5 CKD, kidney failure, a kidney transplant or those interested in living donation. People interested in receiving support or becoming a mentor can complete an online application or email nkfpeers@kidney.org, or call 1-855-NKF-PEERS (855.653.7337).
- NKF Council on Renal Nutrition CKD Kidney Dietitian Directory and the Academy of Nutrition and Dietetics “Find a Nutrition Expert” Database are excellent resources to help patients find a registered dietitian in your area who specializes in kidney disease.
- Kidney Risk Quiz - a tool to aid in early detection of kidney disease.
- Kidney Learning Center - designed for patients to better understand and care for kidney disease, it features educational activities on an array of carefully selected topics by well-known health experts on the subject.
- NKF Online Communities - a safe and supportive place where patients and caregivers can share experiences, ask questions, and get answers related to kidney health, kidney disease, transplantation and living organ donation. Participation is free and anonymous.
References
- Al Raiisi F, Stewart D, Fernandez-Llimos F, Salgado TM, Mohamed MF, Cunningham S. Clinical pharmacy practice in the care of Chronic Kidney Disease patients: a systematic review. Int J Clin Pharm. 2019;41(3):630-666. doi:10.1007/s11096-019-00816-4
- Stemer G, Lemmens-Gruber R. Clinical pharmacy activities in chronic kidney disease and end-stage renal disease patients: a systematic literature review. BMC Nephrol. 2011;12:35. doi:10.1186/1471-2369-12-35
- Johns TS, Yee J, Smith-Jules T, Campbell RC, Bauer C. Interdisciplinary care clinics in chronic kidney disease. BMC Nephrol. 2015;16(1):161. doi:10.1186/s12882-015-0158-6
- Nicoll R, Robertson L, Gemmell E, Sharma P, Black C, Marks A. Models of care for chronic kidney disease: A systematic review. Nephrology (Carlton). 2018;23(5):389-396. doi:10.1111/nep.13198
- Vu A, Nicholas SB, Waterman AD, et al. “Positive Kidney Health”: Implementation and design of a pharmacist-led intervention for patients at risk for development or progression of chronic kidney disease. J Am Pharm Assoc (2003). 2023;63(2):681-689. doi:10.1016/j.japh.2022.11.007
- Gheewala PA, Peterson GM, Zaidi STR, Jose MD, Castelino RL. Australian Community Pharmacists’ Experience of Implementing a Chronic Kidney Disease Risk Assessment Service. Prev Chronic Dis. 2018;15:E81. doi:10.5888/pcd15.170485
- Shlipak MG, Tummalapalli SL, Boulware LE, et al. The case for early identification and intervention of chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2021;99(1):34-47. doi:10.1016/j.kint.2020.10.012
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2021. In: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105(4S):S117-S314. doi:10.1016/j.kint.2023.10.018
- Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation. 2021;143(11):1157-1172. doi:10.1161/CIRCULATIONAHA.120.050686
- Van Der Velde M, Matsushita K, Coresh J, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney International. 2011;79(12):1341-1352. doi:10.1038/ki.2010.536
- Delgado C, Baweja M, Crews DC, et al. A Unifying Approach for GFR Estimation: Recommendations of the NKF-ASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease. American Journal of Kidney Diseases. 2022;79(2):268-288.e1. doi:10.1053/j.ajkd.2021.08.003
- Inker LA, Eneanya ND, Coresh J, et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N Engl J Med. 2021;385(19):1737-1749. doi:10.1056/NEJMoa2102953

