Hemodialysis
- English
- Español
Table of Contents
About Hemodialysis
Hemodialysis is a life-saving treatment for people with kidney failure, which helps your body remove extra fluid and waste products from your blood when the kidneys are not able to.
Uses
Dialysis is helpful for two different situations:
- Acute kidney injury (AKI): a sudden episode of kidney failure or kidney damage that happens within a few hours or days. AKI is usually treated in a hospital setting with intravenous fluids (given through the vein). In severe cases, dialysis may also be needed for a short time until the kidneys get better.
- Kidney failure end-stage kidney disease (ESKD): when 10%-15% of your kidney function remains, measured by an estimated glomerular filtration rate (eGFR) of less than 15 mL/min.
How it works
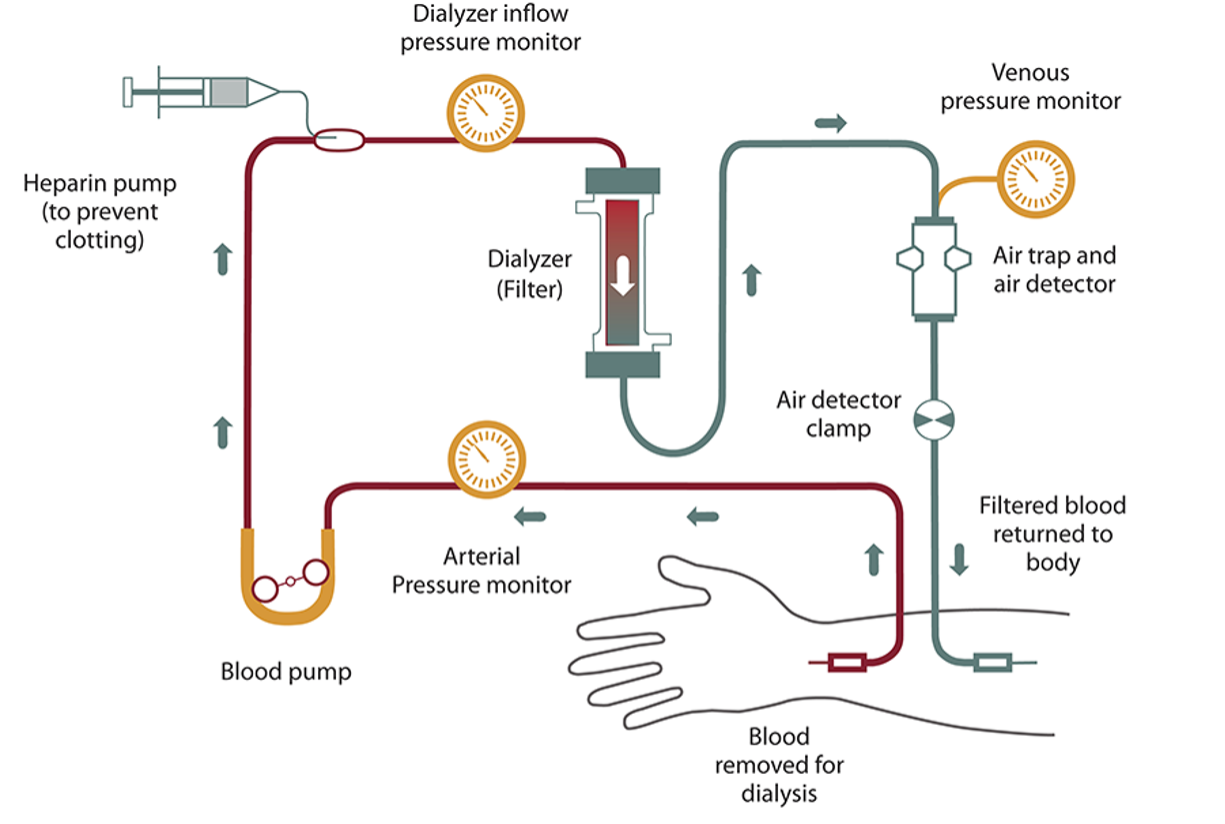
A hemodialysis machine works as an artificial kidney by:
- Removing waste and extra fluids in your body to prevent them from building up in the body
- Keeping safe levels of minerals in your blood, such as potassium, sodium, calcium, and bicarbonate
- Helping to regulate your blood pressure
The machine has a special dialyzer filter to clean your blood. To get your blood to the dialyzer, a surgeon will make an opening into one of your blood vessels. This opening is called a vascular access, and it is done with minor surgery, usually in your arm.
Inside the dialyzer or filter, there are two sides—one for blood and the other for dialysate fluid. A thin film, called a membrane, separates these two sides.
Blood cells, proteins, and types of cells remain in your blood because they are too big to pass through the membrane. Smaller waste products, such as urea and creatinine, and extra fluid, move from your blood through the membrane and are removed.
The composition of the dialysate, or cleansing fluid, is made for your special needs according to your healthcare professional’s prescription.
Types
Hemodialysis can be performed at a hospital, a dialysis center, or at home. Treatments at a dialysis center are usually done 3 times a week, each taking 3 to 4 hours to complete.
Home hemodialysis treatments may be performed more frequently, usually 5 to 6 days a week. You and your healthcare provider should decide where to have your treatment.
Effectiveness
Hemodialysis is a very effective treatment option for clearing waste products and extra fluid from your blood. However, it does not fully replace all of the kidney’s functions, so it is not considered a cure for advanced CKD or kidney failure.
In some cases of sudden AKI, hemodialysis may only be needed for a short time until the kidneys get better. However, when kidney disease progresses slowly to kidney failure, your kidneys do not get better. You will need dialysis for the rest of your life unless you can receive a kidney transplant.
Side effects
Hemodialysis does have side effects. Sometimes, it is hard to tell whether a symptom is due to treatment or if kidney failure is causing discomfort. Some of the most common side effects that people report include:
- Blockage in your vascular access site (entrance point)
- Muscle cramps
- Hypotension (low blood pressure)
- Weakness, dizziness, or nausea
- Blood loss
If you experience symptoms like cramps, headaches, nausea, or dizziness during dialysis, ask your dialysis care team if any of the following steps could help you:
- Slowing down fluid removal may make you feel better but increase the time spent getting treatment.
- Check the dose and timing of your blood pressure medications.
- Adjust your dry weight or target weight.
- Lower the temperature of the dialysate a little.
- Ask your healthcare provider if it would help to change to a different type of dialyzer.
You can help yourself by carefully following your sodium (salt) and fluid limits between treatments to decrease fluid buildup in your body.
Additional considerations
Dietary needs
Your diet will likely be different from the one you followed before starting dialysis. Although certain foods may be limited, you must get enough protein and calories to maintain good health. The kidney dietitian at your center will help you develop a meal plan that meets your needs.
It’s important to keep to your fluid and sodium (salt) limits so you don’t build up too much fluid in your body between treatments. This buildup may lead to needing more fluid removal (ultrafiltration) during your dialysis treatment. Ultrafiltration may cause some discomfort during your treatment. Excess fluid buildup can also increase your blood pressure.
Your daily diet should not include more than 2,000 mg of sodium (salt) to help prevent fluid buildup between treatments. Your kidney dietitian can help you plan a low-sodium diet. You may also need to limit the amount of potassium and phosphorus in your diet. Review your monthly labs with your kidney dietitian and discuss your diet needs.
Health insurance
The federal government’s Medicare program covers 80% of all dialysis costs for most patients. If you are not already on Medicare when you start dialysis, your coverage will start on the 1st day of the 4th month. If you begin a home training program within your first 90 days of treatment, then coverage will be retroactive, which means you will be covered from day 1.
Private insurance or state Medicaid programs may also help with the costs. Ask your social worker or financial coordinator about your insurance options.
Dialysis centers also have billing personnel who can answer your insurance coverage and billing questions.
Travel
Dialysis centers are in every part of the United States and many other countries. Before you travel, you should make an appointment for dialysis treatment at a dialysis center in your destination. The staff at your dialysis center may be able to help you arrange the appointment.
Working
Many people on dialysis continue to work. However, if your job requires a lot of physical labor (heavy lifting, digging, etc.), you may need to change some of your duties.
Questions for your healthcare team
When considering hemodialysis, it’s important to have open and honest conversations with your healthcare team. Here are some questions you might consider asking:
- What are the pros and cons of hemodialysis compared to other types of dialysis? Understanding the benefits and risks of hemodialysis versus peritoneal dialysis or other options can help you make an informed decision.
- How do I know if home hemodialysis is right for me? Discuss the requirements and support available for home hemodialysis to see if this treatment will work with your lifestyle and medical needs.
- What should I expect during my first hemodialysis session? Knowing what happens during the initial session can help lower your anxiety and prepare you for the process.
- How will hemodialysis affect my daily life? Understanding the impact on your routine, work, and social activities can help you plan accordingly.
- What dietary changes will I need to make while on hemodialysis? Specific dietary guidelines are crucial for managing your health on dialysis. Your kidney dietitian can provide tailored advice.
- What are the possible side effects of hemodialysis, and how can they be managed? Knowing the common side effects and management strategies can help you better cope with treatment.
- What happens if I miss a hemodialysis session? Discuss the steps and possible things that can happen when a session is missed so you can stay on track with your treatment.
- What support services are available to me? Learn about counseling, support groups, and other resources to support you during your treatment.
- Can I travel while on hemodialysis? Ask about the planning required for traveling to make sure you can continue your treatment while away from home.
- How will my health insurance cover hemodialysis costs? Understanding your insurance coverage and any out-of-pocket expenses is important for financial planning.
- What should I do if I experience complications or side effects outside of dialysis sessions? Knowing when and how to contact your healthcare team in emergencies can provide peace of mind.
More resources
- Dialysis and You
- Hemodialysis What you need to know - Stage 5
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
- Centers for Disease Control and Prevention (CDC)
- NKF Council on Renal Nutrition CKD Kidney Dietitian Directory
This content is provided for informational use only and is not intended as medical advice or as a substitute for the medical advice of a healthcare professional.
