Last updated: March 07, 2025
Medically reviewed by: NKF Patient Education Team
Before starting home dialysis, your training team will check your home, help set up your treatment space, arrange needed surgery, and provide information on payment options.
Learn about your type of home dialysis
As you prepare to start home dialysis, take time to learn about the type of dialysis you’ve chosen. Understanding how it works, what to expect, and how to manage your treatment at home can help you feel more confident and prepared for your care.
Home hemodialysis
If you choose home hemodialysis, the training center will make sure you know how to:
- Set up the equipment in your home
- Store and order your supplies
- Use and care for your dialysis machine
- Recognize and fix equipment problems or know who to call for help
- Weigh yourself and figure out how much fluid you will need to remove from your blood
- Insert and remove needles from your dialysis access site. Your access site is where your dialysis machine connects to your body to pump your blood.
- Check your blood pressure
- Write down your treatment records
Peritoneal dialysis
If you choose peritoneal dialysis, make sure you know how to:
- Add and drain cleansing fluid through your catheter (the thin, flexible tube in your belly)
- Clean your catheter
- Prevent infections like peritonitis
- Use and care for your dialysis machine (if you choose to do continuous cycling peritoneal dialysis CCPD)
- Recognize and fix CCPD machine problems or know who to call for help
Set up your home treatment space
Your treatment space
Before you start home dialysis, you will need to set up your home treatment space where you will do your treatments. This space can be an area or room in your home that you can keep clean.
- If you have pets, use a room with a door to keep pets out.
- If you choose to do treatments overnight, your bedroom can be used as your treatment space.
Things you may want in your treatment space:
- A comfortable bed or chair to rest or sleep during your treatment
- Good lighting so you and your care partner can set up your treatments
- Entertainment you can easily reach
- Close to the sink
If you choose home hemodialysis, your treatment space may need these for your dialysis machine:
- A grounded electrical outlet
- Access to water
- A drain or other plumbing to get rid of treatment fluids
Your supplies
You will also need an area or closet to store your supplies. You will need enough space to store at least 6 weeks of supplies at a time.
These supplies can take up a lot of space. To save space you can:
- Stack supplies that are in sturdy boxes
- Remove supplies from boxes to store in baskets, drawers, or shelves (do not remove supplies from any sterile, sealed packaging)
Your home dialysis nurse will make a home visit as part of your home treatment training. They can help you set up your treatment and storage space.
Have surgery to create an access point
Home hemodialysis
If you choose home hemodialysis, you will have surgery before you can start. This is to create an access site for the home dialysis machine to connect to your body to pump your blood.
You will have 1 of these 3 types of surgeries for home hemodialysis:
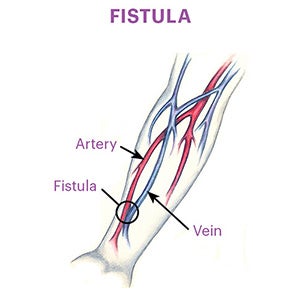
Fistula – A surgeon connects an artery in your forearm and a nearby vein to create an access site. This is the first choice for most people as it has fewer problems and is the longest lasting than a graft or catheter.
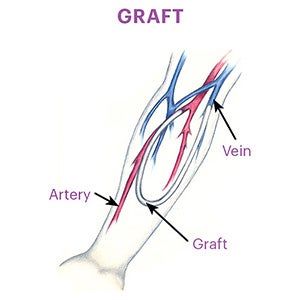
Graft – A surgeon connects an artery and a nearby vein with a small tube to create an access site. This is a second option if a fistula isn’t possible. It is more likely to get infected or to clot than a fistula, which may need treatment or surgery to fix or replace.
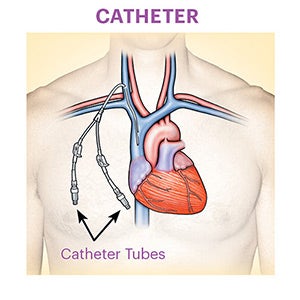
Catheter – A surgeon puts a catheter (a thin, flexible tube) into a large vein in your neck or chest. Surgeons will only do this if you will be on dialysis for a long time and they cannot do a fistula or graft. It is more likely than the fistula or graft to get infections and clots. If you have this surgery, you will need to follow strict care instructions for the catheter.
Peritoneal dialysis
If you choose peritoneal dialysis, you will have surgery so a surgeon can place a catheter (a thin, flexible tube) in your belly. This lets you use the special cleaning fluid (dialysate) to clean your blood.
Learn how you will pay for home dialysis
Your dialysis center social worker can help you learn more about coverage, costs, and how to pay for them.
Medicare
If you have kidney failure, you may qualify for Medicare. Medicare can pay for a large amount of home dialysis, including:
- Home dialysis training for you and your care partner
- Equipment and supplies
- Support services such as visits from a home dialysis nurse to check you or your equipment
- Lab tests or medicines related to dialysis or kidney failure
- Private insurance
- Some managed care organizations
- Medicaid
- Veterans Administration (VA)
- Indian Health Services (IHS)
Private insurance
If you currently have insurance through your employer, they will pay for the first 30 months of home dialysis. Then, if you apply and qualify, Medicare will become your primary coverage and pay 80% of home dialysis costs. You will have to pay the remaining 20%.
There are other groups that can help you pay the remaining costs, such as:
- Private insurance
- Some managed care organizations
- Medicaid
- Veterans Administration (VA)
- Indian Health Services (IHS)
Other home dialysis costs
If you choose to do home hemodialysis, you may need plumbing or wiring changes in your home so your machine can work properly. These costs may be covered by your private insurance. However, newer machines have standard outlets, so you may not need to do this.
You may also have a higher water and electric or gas bills because of your dialysis machine.








